Fibromyalgia, a chronic condition affecting 1 in 20 people in the UK, causes widespread pain, fatigue, sleep disturbances, and cognitive issues. Conventional treatments often fail to provide sufficient relief, leaving many to explore alternatives like medical cannabis. Legal since 1 November 2018 in the UK for those who have exhausted other options, medical cannabis has shown promising results, including a 77% reduction in pain and 78% improvement in sleep quality among patients.
If you’re considering medical cannabis for fibromyalgia, here’s a quick checklist to determine your eligibility:
- Confirmed Diagnosis: You must have an official fibromyalgia diagnosis from a GP or specialist.
- Tried Conventional Treatments: Medical cannabis is typically prescribed after at least two standard treatments fail, such as amitriptyline, pregabalin, or physiotherapy.
- No Red Flags in Medical History: Conditions like psychosis, severe heart disease, or pregnancy may disqualify you.
- Clear Treatment Goals: Whether it’s reducing pain, improving sleep, or cutting back on opioids, having defined objectives is essential.
While NHS prescriptions remain rare, private clinics offer consultations and access to cannabis-based medicinal products (CBMPs). Treatment involves tailored plans, starting with low doses, and products like oils, capsules, or vapourised flower. Side effects, such as fatigue or dry mouth, are generally mild but should be monitored.
Cost Consideration: Private treatment costs include consultation fees (~£99) and monthly medication expenses, which vary by product and dosage.
Medical cannabis isn’t a cure but can help manage symptoms. If you meet the criteria, book a consultation with a specialist to explore this option further.
Fibromyalgia and Medical Cannabis: The Basics
What Is Fibromyalgia?
Fibromyalgia syndrome (FMS) is a long-term condition that affects how the central nervous system processes pain. Unlike pain that’s confined to a specific area, fibromyalgia causes widespread discomfort across various parts of the body for at least three months.
People living with fibromyalgia often endure more than just persistent pain. It’s common to experience extreme fatigue, difficulty sleeping, and cognitive challenges – often referred to as “fibro fog.” Some individuals also report gastrointestinal symptoms.
Experts believe fibromyalgia may be linked to abnormal levels of brain chemicals and changes in how pain signals are processed by the nervous system. Another theory, known as Clinical Endocannabinoid Deficiency (CECD), suggests that a lack of naturally occurring endocannabinoids in the body could play a role. These potential imbalances in pain signalling and the endocannabinoid system have sparked interest in cannabis-based treatments as a possible solution.
Why Consider Medical Cannabis?
For those who find little relief or face significant side effects with conventional treatments, medical cannabis offers an alternative worth exploring. Cannabis-based medicinal products (CBMPs) interact with the body’s endocannabinoid system (ECS), which influences pain, sleep, and mood regulation.
The two key compounds in cannabis, THC (delta-9-tetrahydrocannabinol) and CBD (cannabidiol), work in different ways. THC primarily binds to CB1 receptors in the central nervous system, altering how pain signals are processed. CBD, on the other hand, interacts with CB2 receptors in immune cells and is thought to enhance the effects of the body’s own endocannabinoids.
“Research indicates that cannabis may affect the endocannabinoid system, which plays a role in pain perception, sleep regulation and mood.” – Dr Hanna Gul, Rheumatology Specialist
These interactions make cannabis an intriguing option for managing fibromyalgia’s complex symptoms.
What Does the Research Say?
Recent studies from the UK Medical Cannabis Registry provide encouraging data. A July 2023 study by Imperial College London, which followed 306 patients, and earlier research from May 2022 led by Dr Simon Erridge and Dr Wendy Holden, revealed significant improvements in quality of life and sleep at 1-, 3-, 6-, and 12-month intervals. Additionally, there was a 17% reduction in opioid use within the first month of treatment.
“CBMP treatment was associated with improvements in fibromyalgia-specific symptoms, in addition to sleep, anxiety, and health-related quality of life… CBMPs were generally well-tolerated.” – Wang, C. et al., UK Medical Cannabis Registry Researchers
Despite these positive findings, large-scale randomised controlled trials are still lacking. Currently, CBMPs are unlicensed for fibromyalgia in the UK and are only prescribed by specialist consultants on a case-by-case basis. The most common side effects include fatigue (24.51%), dry mouth (22.55%), and difficulty concentrating (21.57%), though most reported adverse effects are mild to moderate.
A Discussion of Cannabis Medicines and CBD for Fibromyalgia and Arthritis – Part 1
Eligibility Checklist: Are You a Suitable Candidate?
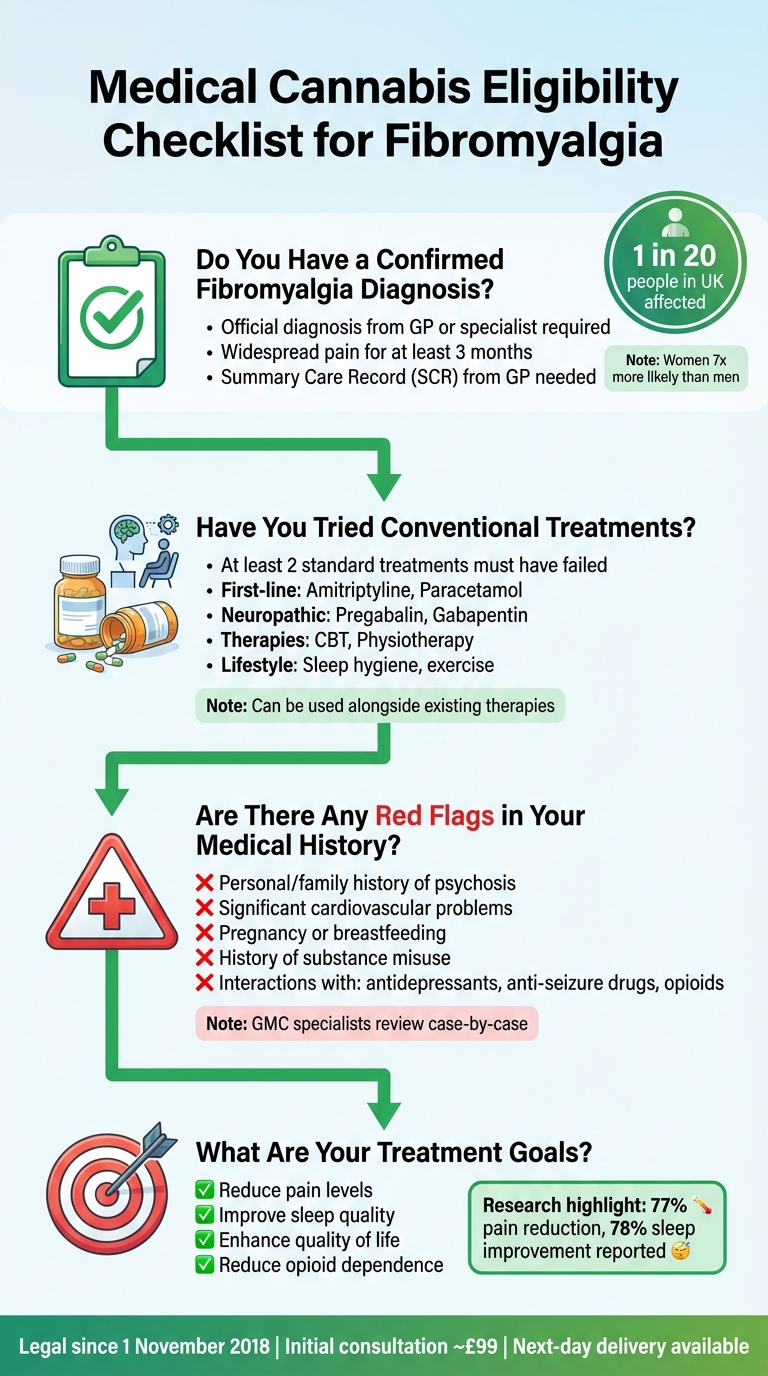
Medical Cannabis Eligibility Checklist for Fibromyalgia Patients in UK
Wondering if you qualify for medical cannabis treatment? This checklist breaks down the essential requirements and considerations to help you decide.
Do You Have a Confirmed Fibromyalgia Diagnosis?
To legally access medical cannabis in the UK, you must have a formal diagnosis of fibromyalgia from your GP or a specialist, such as a rheumatologist. This diagnosis should align with nationally recognised criteria, which include experiencing widespread pain for at least three months and ruling out other potential conditions through appropriate tests.
“Fibromyalgia is a chronic condition characterised by widespread pain, fatigue, sleep disturbances and cognitive difficulties. Managing fibromyalgia can be a challenge due to the complexity and variability of symptoms.” – Dr Hanna Gul, Rheumatology Specialist
You’ll also need to provide a Summary Care Record (SCR) from your GP, which confirms your diagnosis and medical history. This document is vital for your consultation at a private clinic, so contact your GP surgery to request it in advance.
Medical cannabis may offer relief from a range of fibromyalgia symptoms, not just pain. It can also address issues like ‘fibro fog’ (cognitive difficulties), muscle stiffness, headaches, irritable bowel syndrome, and anxiety. Did you know that fibromyalgia affects about 1 in 20 people in the UK, with women being seven times more likely to develop it than men?.
Once your diagnosis is confirmed, take a closer look at your previous treatments to see if medical cannabis could be the next step for you.
Have You Tried Conventional Treatments?
In the UK, medical cannabis is typically considered a second-line treatment. This means you’ll usually need to have tried at least two conventional medications without seeing enough improvement.
“Medical cannabis is only prescribed when conventional treatments have been exhausted or to complement existing therapies.” – Elios Clinics
Here’s a quick overview of common first-line treatments for fibromyalgia:
- First-line Medications: Amitriptyline, Paracetamol
- Neuropathic Drugs: Pregabalin, Gabapentin
- Therapies: Cognitive Behavioural Therapy (CBT), Physiotherapy
- Lifestyle Adjustments: Sleep hygiene, regular exercise
Prepare a clear record of the treatments you’ve tried and why they didn’t work. While your SCR will include much of this information, keeping your own symptom diary can be incredibly helpful. Track details like pain levels, flare-ups, and sleep quality to provide extra evidence during your consultation. Remember, medical cannabis can often be used alongside existing therapies rather than replacing them entirely.
Are There Any Red Flags in Your Medical History?
Certain pre-existing conditions might require extra caution or could even disqualify you from treatment. Specialists registered with the GMC will review your SCR and assess your eligibility on a case-by-case basis.
“People with certain medical conditions such as epilepsy, heart disease, or HIV should not take medical cannabis without consulting a doctor.” – Elios Clinics
Some key factors that could affect your eligibility include:
- Personal or family history of psychosis or severe mental health issues
- Significant cardiovascular problems, as cannabis can elevate heart rate
- Pregnancy or breastfeeding
- History of substance misuse (some clinics have addiction specialists to handle these cases safely)
Be transparent about all medications you’re currently taking, as cannabis can interact with antidepressants, anti-seizure drugs, and opioids. If you have a history of heart disease, discuss the potential risks with your doctor before starting treatment.
Once you’ve clarified your medical history, it’s time to focus on what you’d like to achieve with treatment.
What Are Your Treatment Goals?
Think about what you want to get out of medical cannabis treatment. Are you looking to reduce pain, improve sleep, or enhance your overall quality of life? Maybe your goal is to cut back on opioids or other medications with difficult side effects.
Evidence suggests that many fibromyalgia patients experience better pain management and improved sleep with medical cannabis. Setting clear, realistic goals will help your specialist create a treatment plan tailored to your needs. Keep in mind, medical cannabis isn’t a cure – it’s a tool to help manage symptoms and make daily life more manageable.
sbb-itb-24979b8
What to Expect from Cannabis Treatment
Once you’ve confirmed eligibility, it’s time to dive into the practical aspects of medical cannabis treatment – this includes understanding the types of products available, how treatment is administered, potential risks, and the associated costs. Here’s a closer look at what you can expect.
What Types of Cannabis-Based Products Are Available?
Cannabis-based medicinal products (CBMPs) come in a variety of forms, each designed to suit different needs and methods of use. Oils and tinctures, taken under the tongue, are commonly used for pain relief and sleep issues, providing effects that last 6–8 hours. Dried flower, on the other hand, is vapourised with a medical device for fast-acting relief – effects begin within 1–5 minutes but wear off after 2–4 hours. For those seeking longer-lasting effects, capsules can provide relief for over eight hours, though they take 1–2 hours to kick in. Meanwhile, topical patches and creams are ideal for targeting localised muscle stiffness without affecting the rest of your body.
Products are also classified by their cannabinoid content. High-THC formulations primarily interact with CB1 receptors in the brain and spinal cord, helping to manage pain and mood. In contrast, high-CBD products focus on CB2 receptors, which are more involved in reducing inflammation. There are also balanced THC:CBD products, which combine the benefits of both. For example, a Dutch study found that a balanced strain (Bediol) reduced pain levels by 30% in 90% of participants. A 2024 cohort study further highlighted the effectiveness of oils, dried flower, and combinations of products in managing fibromyalgia symptoms, suggesting that the best choice often depends on your lifestyle and specific symptoms.
How Is Treatment Administered?
Treatment is highly personalised, starting with a “start low, go slow” approach. This means beginning with a small dose and gradually increasing it to find the right balance between symptom relief and side effects. Since everyone’s endocannabinoid system is different, there’s no one-size-fits-all dosage – your plan will be tailored to factors like your symptoms, body weight, and how you’ve responded to treatments in the past. For instance, an Israeli study revealed that patients experienced a significant drop in pain intensity, from an average of 9/10 to 5/10, when their cannabis treatment was carefully adjusted.
For those dealing with sleep disturbances or muscle spasms, dosing is often scheduled in the evening to take advantage of the sedative properties of certain strains. Importantly, medical cannabis should never be smoked; vapourising dried flower with a medical device is the recommended method, both for health reasons and to comply with legal guidelines.
What Are the Risks and Side Effects?
Like any treatment, medical cannabis comes with potential side effects. Common short-term issues include dry mouth, dizziness, drowsiness, nausea, headaches, and changes in appetite or weight. Some people may also experience psychological effects like increased anxiety, panic, or paranoia, particularly when using high-THC products. An elevated heart rate is another possible side effect, which is why cannabis treatment may not be suitable for those with serious heart conditions.
In a UK Medical Cannabis Registry study involving 148 fibromyalgia patients, 24.32% reported adverse effects, with new users being more likely to encounter side effects. On the positive side, about 20% of participants in a clinical study were able to significantly reduce or stop using medications like benzodiazepines or opioids after incorporating cannabis into their treatment plan. However, any changes to existing medications should only be made under the guidance of a specialist. And remember, driving while under the influence of cannabis is illegal.
Being aware of these risks helps you manage expectations and make informed decisions about your treatment.
What Are the Costs?
The cost of medical cannabis treatment varies depending on your specific plan. Unfortunately, it is rarely available on the NHS for conditions like fibromyalgia, as NICE considers it not cost-effective due to the high expense compared to its modest benefits. For private treatment, you’ll need to budget for an initial consultation (typically around £99), follow-up appointments, and the monthly cost of medication, which depends on the product and dosage.
Some clinics offer monthly packages or memberships to help make treatment more affordable, so it’s worth comparing options as part of your research. This can help you find a plan that works for both your needs and your budget.
How Elios Clinics Can Support Your Journey
Elios Clinics is dedicated to guiding patients through every stage of their fibromyalgia treatment, offering a patient-focused approach that prioritises care and support.
Eligibility Assessments and Consultations
Start your journey with a free eligibility check available on the Elios Clinics website. This step confirms whether you’re suitable for treatment. If eligible, you’ll be scheduled for a video consultation with a specialist doctor registered with the GMC Specialist Register. These doctors are authorised to prescribe medical cannabis in the UK. During this initial meeting, the doctor will review your medical history, discuss your symptoms in detail, and collaborate with you to create a treatment plan tailored to your needs. Medical cannabis will only be prescribed if conventional treatments have been tried without success or if it will complement existing therapies. This personalised approach ensures a strong foundation for your ongoing care.
Ongoing Support and Monitoring
Your treatment journey doesn’t stop with the first prescription. Elios Clinics offers regular follow-up consultations to track your progress and adapt your treatment as needed. These structured appointments ensure your care evolves alongside your symptoms. Through the online patient dashboard, you can manage prescriptions, book appointments, and request repeat medications, all with the convenience of next-day delivery. Clinicians stay actively involved, monitoring your progress and making adjustments to optimise your outcomes. This continuous care reflects the clinic’s dedication to your well-being.
Commitment to Safety and Quality
Safety is a top priority at Elios Clinics. The clinic strictly adheres to UK regulations that have been in place since medical cannabis was legalised in 2018. Every treatment is prescribed by GMC-registered specialist doctors. Before beginning treatment, clinicians thoroughly review your medical history to rule out any contraindications, such as heart disease, epilepsy, HIV, or pregnancy and breastfeeding, which could make cannabis unsuitable. Additionally, the clinic ensures that all cannabis-based medicinal products meet rigorous quality standards. As the clinic explains:
“At Elios Clinics, we are happy to help our patients obtain a private prescription and get the medication legally. We understand the importance of taking all the necessary steps to ensure that cannabis is used responsibly”.
Conclusion
To determine if medical cannabis might be right for managing your fibromyalgia, start by reviewing your diagnosis, previous treatments, and personal health objectives. Use this checklist as a guide to evaluate whether you meet the clinical criteria currently recognised in the UK. While this is a helpful starting point, it’s only the first step.
It’s important to emphasise that a checklist cannot replace professional medical advice. Consulting a specialist is crucial to ensure medical cannabis is both safe and suitable for your unique needs. Specialists can assess potential contraindications, create a tailored treatment plan, and provide ongoing monitoring to help you achieve the best possible results. This personalised approach complements earlier strategies for managing fibromyalgia and highlights the potential role of medical cannabis.
If you believe you meet the necessary criteria, you can take the next step by scheduling a free eligibility assessment through the Elios Clinics website. Be sure to prepare your medical records and symptom notes in advance to make your consultation as productive as possible.
FAQs
Can medical cannabis be used alongside traditional fibromyalgia treatments?
Medical cannabis is sometimes viewed as an alternative when traditional treatments like painkillers or antidepressants aren’t providing enough relief. It interacts with the endocannabinoid system, which plays a role in easing pain and supporting better sleep patterns.
In some cases, using medical cannabis might lower the need for higher doses of standard medications, which could, in turn, reduce unwanted side effects. If you’re thinking about exploring this option, it’s important to consult a specialist who can assess whether it fits your symptoms and treatment plan.
What side effects might occur when using medical cannabis for fibromyalgia?
Medical cannabis has been found to assist in managing fibromyalgia symptoms, but it’s not without potential side effects. Some of the more common ones include dry mouth, which can be alleviated by drinking plenty of water and using sugar-free gum, and dizziness, particularly when getting up too quickly. Changes in appetite are also possible – THC might make you feel hungrier, while CBD could have the opposite effect. Other side effects may involve daytime drowsiness or difficulty focusing, which often occur if the dosage isn’t quite right. For those using high-THC products, there’s also the possibility of experiencing anxiety, and there’s always the chance of interactions with other medications, making professional oversight essential.
To reduce the likelihood of these side effects, starting with a low dose and carefully observing your body’s response is key. At Elios Clinics, patients benefit from tailored guidance and expert support, ensuring their treatment plan is both effective and safe, striking the right balance between symptom management and overall comfort.
Is medical cannabis available on the NHS for treating fibromyalgia?
No, medical cannabis is not currently offered through the NHS for treating fibromyalgia. According to the National Institute for Health and Care Excellence (NICE), these treatments are not considered a cost-effective use of NHS resources and are recommended only within the context of clinical trials.
For those considering medical cannabis, private clinics such as Elios Clinics can evaluate your suitability and offer personalised treatment plans for fibromyalgia and other chronic conditions.