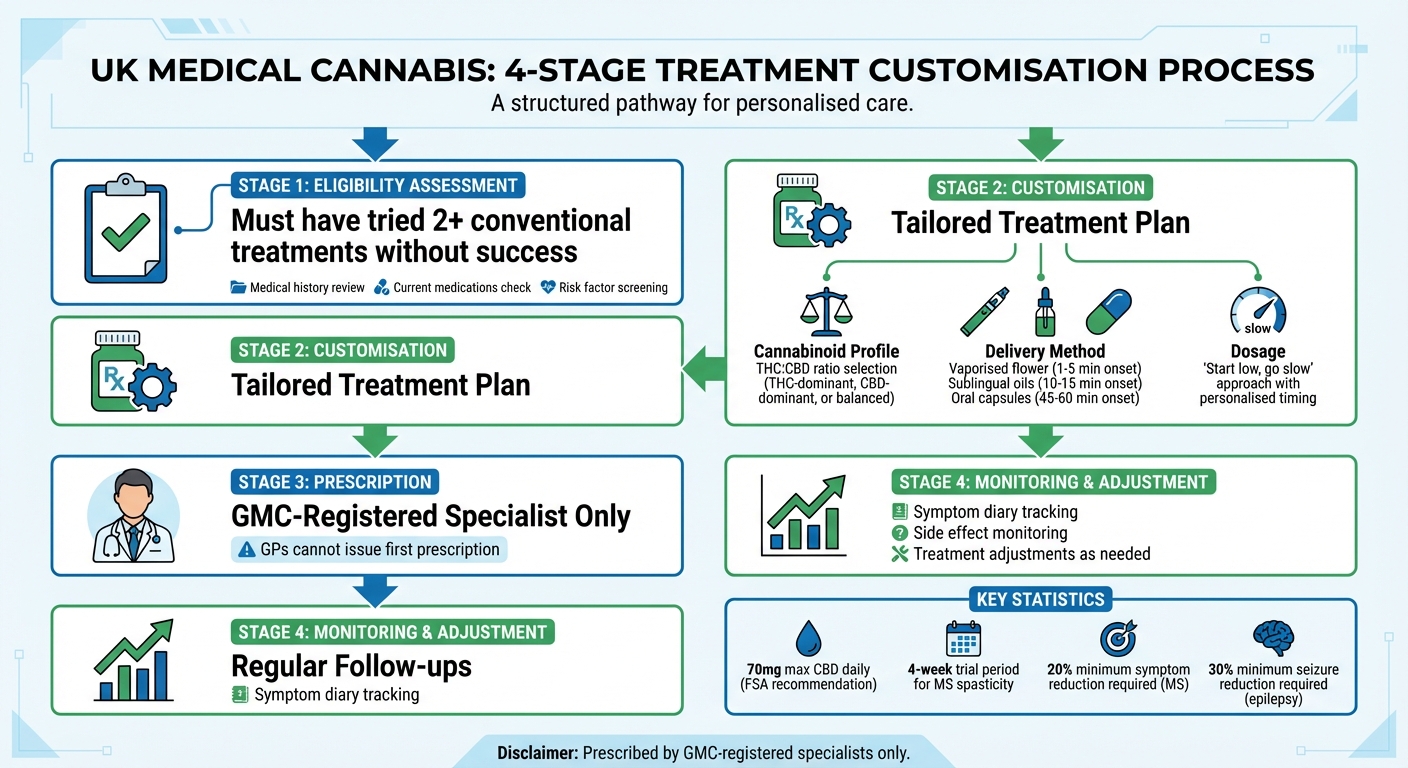
Medical cannabis treatments in the UK are tailored to individual needs. Doctors consider your condition, symptoms, medical history, and how your body reacts to treatment. Unlike over-the-counter CBD, prescribed cannabis products may contain THC and are strictly regulated. Here’s how personalisation works:
- Eligibility: You must have tried at least two conventional treatments without success.
- Assessment: Doctors review your medical history, current medications, and risk factors like mental health or substance misuse.
- Customisation: Treatment plans focus on the right THC:CBD ratio, delivery method (e.g., oils, capsules, vapour), and dosage schedule.
- Monitoring: Regular follow-ups ensure the treatment is adjusted based on your progress and side effects.
Prescriptions are issued only by specialists registered with the GMC. This personalised approach ensures safe and effective use of cannabis-based medicines for conditions like chronic pain, epilepsy, and MS-related spasticity.
Medical Cannabis Treatment Customisation Process in the UK
How Doctors Assess Patient Eligibility
Before prescribing medical cannabis, doctors follow a structured assessment process to ensure it is both safe and appropriate under UK regulations. This thorough evaluation helps determine whether cannabis-based medicines are a suitable option for a patient’s condition.
Medical History and Treatment Review
A comprehensive review of the patient’s medical history forms the basis for creating a personalised treatment plan. Doctors examine the patient’s diagnosis, the severity of symptoms, and how these affect daily life. They also evaluate any current medications to identify potential interactions, such as with central nervous system depressants, antiepileptics, or hormonal contraceptives. Additionally, physical health factors like liver, kidney, and cardiovascular function are assessed to understand how the body might process cannabis-based treatments.
Patients are encouraged to disclose any use of over-the-counter or illicit cannabis products. This information is crucial, as stopping these products may be necessary before starting a regulated prescription. Such transparency ensures doctors have a complete understanding of the patient’s circumstances, enabling informed and safe treatment decisions.
UK Eligibility Requirements
In the UK, patients must typically have tried at least two conventional licensed treatments that either failed to alleviate their condition or caused intolerable side effects. Known as the "two-treatment rule", this requirement ensures that cannabis-based medicines are considered only after other options have proven ineffective. Patients are required to provide documentation of these prior treatments.
"Initial prescription of cannabis-based medicinal products… must be made by a specialist medical practitioner (a doctor included in the register of specialist medical practitioners)." – NICE
This rule ensures that only patients with documented treatment resistance are eligible for medical cannabis. Furthermore, only specialists listed on the GMC Specialist Register can initiate prescriptions for unlicensed cannabis-based products. General practitioners are not authorised to issue the first prescription. The prescribing specialist must also have expertise in the relevant condition, such as a neurologist for epilepsy or a pain specialist for chronic neuropathic pain.
Evaluating Patient Risk Factors
Doctors also assess various risk factors to ensure patient safety. A detailed mental health history is reviewed, particularly to screen for conditions like psychosis, which may be exacerbated by THC-containing products. A history of substance misuse, including illicit cannabis use, is also considered to evaluate the risk of dependence or misuse.
Certain groups face additional restrictions. For example, breastfeeding patients are advised against using some licensed products, and there is limited safety data on cannabis use during pregnancy. In children, the potential impact of THC on brain development is a significant concern. Patients with severe liver, kidney, or cardiovascular conditions may also be deemed unsuitable for cannabis-based treatments due to safety risks.
How Doctors Customise Cannabis Treatments
When a patient is deemed eligible for medical cannabis, doctors develop a tailored treatment plan by fine-tuning three main factors: the cannabinoid profile, the delivery method, and the dosage schedule. These adjustments are guided by the patient’s medical history, current condition, and how they respond to the treatment.
Choosing the Right Cannabinoid Profile
Doctors carefully select a cannabinoid profile that aligns with the patient’s specific needs. This can involve a THC-dominant, CBD-dominant, or balanced THC:CBD profile, depending on the condition and the patient’s tolerance. For example:
- Severe epilepsy: Pure CBD products, like Epidyolex, are often prescribed for treatment-resistant epilepsies, especially in younger patients. This is because THC’s safety in developing brains remains uncertain.
- Multiple sclerosis: Patients with moderate to severe spasticity may benefit from a balanced THC:CBD profile, such as Sativex spray, particularly when other treatments have failed.
- Chronic pain: The choice of cannabinoid ratios depends on the type of pain and the patient’s response to previous medications.
- Psychiatric conditions: Patients with a history of psychosis or schizophrenia are generally advised to avoid THC-dominant profiles.
Selecting the Delivery Method
The delivery method is chosen based on how quickly relief is needed and how long the effects are required to last. Common options include vaporised flower, oils, capsules, and sprays:
- Vaporised flower: Offers the quickest relief, with effects starting in 1–5 minutes and lasting 2–4 hours.
- Sublingual tinctures: Takes 10–15 minutes to take effect, with relief lasting 4–6 hours, as the liver is bypassed.
- Oral capsules: These take 45–60 minutes to work but provide relief for 6–8+ hours. This is due to the liver converting THC into a more potent compound, 11-hydroxy-delta-9-THC.
In the UK, smoking medical cannabis is strictly prohibited. Instead, inhalation methods involve vaporisation using approved devices. The choice of delivery method often varies depending on the patient’s condition and individual circumstances.
Determining Dose and Timing
After selecting the delivery method, doctors focus on finding the right dose and timing for the patient.
A "start low, go slow" approach is typically used, beginning with the smallest effective dose to minimise side effects while achieving therapeutic benefits. For conditions like multiple sclerosis-related spasticity, a 4-week trial period is standard to evaluate the treatment’s effectiveness before considering long-term use. Additionally, the Food Standards Agency recommends that healthy adults should not exceed 70mg of CBD per day.
Dosing schedules are customised to suit the patient’s routine and any high-risk periods. Doctors keep detailed records of doses and timings, continuously monitoring for effectiveness and potential side effects, such as drowsiness, dry mouth, or impaired motor skills.
Monitoring and Adjusting Treatment Over Time
Once a tailored treatment plan is in place, doctors don’t just stop there – they continuously refine the therapy based on how the patient responds. Regular follow-ups, whether in person, over the phone, or via video calls, allow doctors to assess how well the treatment is working and make adjustments as needed. This ensures the plan evolves alongside the patient’s needs.
Recording Symptoms and Side Effects
Patients play a key role in this process by keeping a symptom diary. This diary helps track changes in symptoms, the timing of side effects, and any noticeable improvements. Doctors rely on this detailed feedback to evaluate whether the treatment remains both safe and effective. Clinical thresholds are used to measure progress and guide decisions.
"The prescribing doctor has responsibility for… continuing to monitor the effectiveness and side-effects of the prescribed medicine." – Care Quality Commission
In addition to logging symptoms, patients are encouraged to report any changes in their health, new medications they might be taking, or even non-prescribed cannabis use. This information provides doctors with a clearer picture when considering treatment adjustments.
Adjusting Treatment
If the treatment isn’t delivering the desired results or is causing unwanted side effects, adjustments are made. These might include changing the THC:CBD ratio, switching to a different product, or altering the dosage schedule. The aim is always to find the lowest dose that provides maximum benefits while keeping side effects to a minimum.
"Efficacy and safety of cannabis-based medicinal products should be monitored and evaluated, and doses should be adjusted by the initiating specialist prescriber." – NICE
While specialists typically initiate treatment, ongoing dose adjustments can often be managed under shared care agreements between specialists and general practitioners (GPs). These agreements outline how frequently monitoring should occur and the conditions under which treatment might be discontinued.
Working with Medical Teams for Complex Cases
For patients with more complex medical histories or those who don’t respond well to standard treatments, a multidisciplinary team may step in to review the case. These reviews take a holistic approach, addressing all aspects of the patient’s health. When treatments deviate from national guidelines, shared decision-making with other specialists ensures the plan remains both appropriate and safe. If needed, patients might be referred to other healthcare professionals for additional support or alternative treatment options.
sbb-itb-24979b8
Safety Measures and Patient Responsibilities
Doctors adhere to strict safety protocols when prescribing medical cannabis, including thorough assessments of liver, kidney, and cardiovascular health, as well as screening for any history of substance misuse or dependence. Mental health evaluations are especially critical, given the potential impact of THC on brain development and mental health.
"There is evidence that chronic high exposure to THC during recreational cannabis use can affect brain development, structure, and mental health." – NHS England
Breastfeeding is specifically contraindicated for licensed products such as Sativex and nabilone. Patients are also informed about UK driving laws and the legal risks of travelling abroad with controlled substances.
Safety Checks and Contraindications
Doctors undertake comprehensive checks to ensure medical cannabis is safe for each patient. These include:
| Risk Category | What Doctors Check |
|---|---|
| Medical History | Liver or kidney impairment, cardiovascular conditions |
| Psychological Factors | History of psychosis, risk of dependence, effects on brain development (particularly in younger patients) |
| Drug Interactions | CNS depressants, antiepileptics, hormonal contraceptives |
| Lifestyle and Legal Considerations | UK driving laws, international travel restrictions, prohibition on sharing prescribed medicine |
These assessments guide the continuation of treatment, which depends on measurable improvements in symptoms. For instance, patients with multiple sclerosis spasticity must show at least a 20% reduction in symptoms after a four-week trial. Similarly, those with severe epilepsy must experience a minimum 30% reduction in seizure frequency compared to the six months prior to starting treatment.
What Patients Need to Do
Patients play a key role in ensuring their treatment is effective and safe. It is essential to stop using any non-prescribed cannabis – whether illicit, over-the-counter, or online – once medical treatment begins. Prescribed medicine should never be shared with others and must be stored securely.
Patients are encouraged to report any side effects to their healthcare team and through the MHRA Yellow Card Scheme. Additionally, they should disclose all current medications, any changes in their health, and past cannabis use to help prevent adverse interactions.
Understanding Risks and Benefits
Before treatment begins, doctors ensure patients fully understand both the potential risks and benefits. They explain that many cannabis-based products are unlicensed, with limited long-term safety data available, and discuss potential harms and the risk of dependence.
"Because there is a lack of evidence on the long-term safety and effectiveness of cannabis-based medicinal products, clinicians will need to justify prescribing them." – Care Quality Commission
Patients are actively involved in the decision-making process, recognising that most cannabis-based treatments have not undergone the same rigorous testing as licensed medicines. This open dialogue ensures they are aware of the limitations and potential benefits of their treatment before proceeding.
Conclusion
Personalised medical cannabis treatment plans are becoming a key part of how doctors manage chronic conditions. By fine-tuning cannabinoid profiles, delivery methods, and dosages, clinicians aim to enhance treatment results while minimising side effects.
"By tailoring your treatment plan to your unique needs, we can help you achieve better health outcomes and improve your overall quality of life." – Elios Clinics
This patient-focused approach is supported by consistent clinical oversight. With regular 30-day prescriptions and follow-up appointments, doctors can adjust treatments based on real-time patient feedback. This adaptability helps maintain the balance of the endocannabinoid system, which plays a crucial role in regulating sleep, anxiety, movement, and pain.
Patients play an active role by tracking symptoms and sharing updates. This teamwork, guided by specialists registered with the GMC Specialist Register, ensures treatment remains safe, effective, and aligned with lifestyle needs. The combination of specialist knowledge, tailored dosing, and close monitoring creates a comprehensive approach to achieving better outcomes while prioritising safety.
FAQs
Who is eligible for medical cannabis treatment in the UK?
In the UK, medical cannabis can be prescribed for specific conditions, including chronic pain, severe epilepsy that doesn’t respond to treatment, spasticity (such as that caused by multiple sclerosis), or persistent nausea and vomiting. However, it’s not a first-line treatment. Patients must have already tried at least two conventional therapies under the guidance of a specialist, without achieving the desired results.
A medical professional assesses each case individually to ensure the treatment aligns with the patient’s unique circumstances and needs.
How do doctors decide the right balance of THC and CBD for a patient?
Doctors carefully adjust the levels of THC and CBD to suit each patient’s unique needs, considering their symptoms, medical history, and treatment goals. THC is well-known for its ability to relieve pain and relax muscles, though it can produce a psychoactive ‘high’. On the other hand, CBD is non-intoxicating and is often used to address anxiety, inflammation, and nausea. It also helps to balance out some of THC’s effects.
During consultations, doctors take a detailed look at factors like the type of pain, mood, sleep issues, neurological symptoms, and how sensitive the patient might be to psychoactive substances. For those who need pain relief but want to avoid intoxication, a high-CBD and low-THC ratio (such as 1:20) could be suggested. In contrast, conditions like spasticity from multiple sclerosis or severe chronic pain might benefit more from a balanced or THC-dominant ratio, such as 1:1 or 2:1.
These ratios are then incorporated into a personalised treatment plan, which can be adjusted during follow-up appointments. This adaptable approach ensures that the treatment not only provides effective symptom relief but also keeps side effects to a minimum.
Are there any risks of using medical cannabis during pregnancy or while breastfeeding?
The use of medical cannabis during pregnancy or breastfeeding is typically discouraged because of the possible risks it poses to the baby. Studies indicate that compounds found in cannabis, like THC, can cross the placenta or be transferred through breast milk, potentially impacting a baby’s growth and overall health.
If you are pregnant, breastfeeding, or planning to conceive, it’s crucial to consult a qualified healthcare professional. They can offer tailored guidance based on your situation, prioritising the well-being of both you and your baby.
