Medical cannabis and recreational cannabis serve very different purposes, especially in the UK. Medical cannabis is legally prescribed by specialists to manage specific health conditions like chronic pain, epilepsy, or multiple sclerosis. It’s produced under strict pharmaceutical standards to ensure consistent quality, dosage, and safety. Recreational cannabis, however, is illegal, unregulated, and used for personal enjoyment, often prioritising THC potency without medical oversight.
Key differences include:
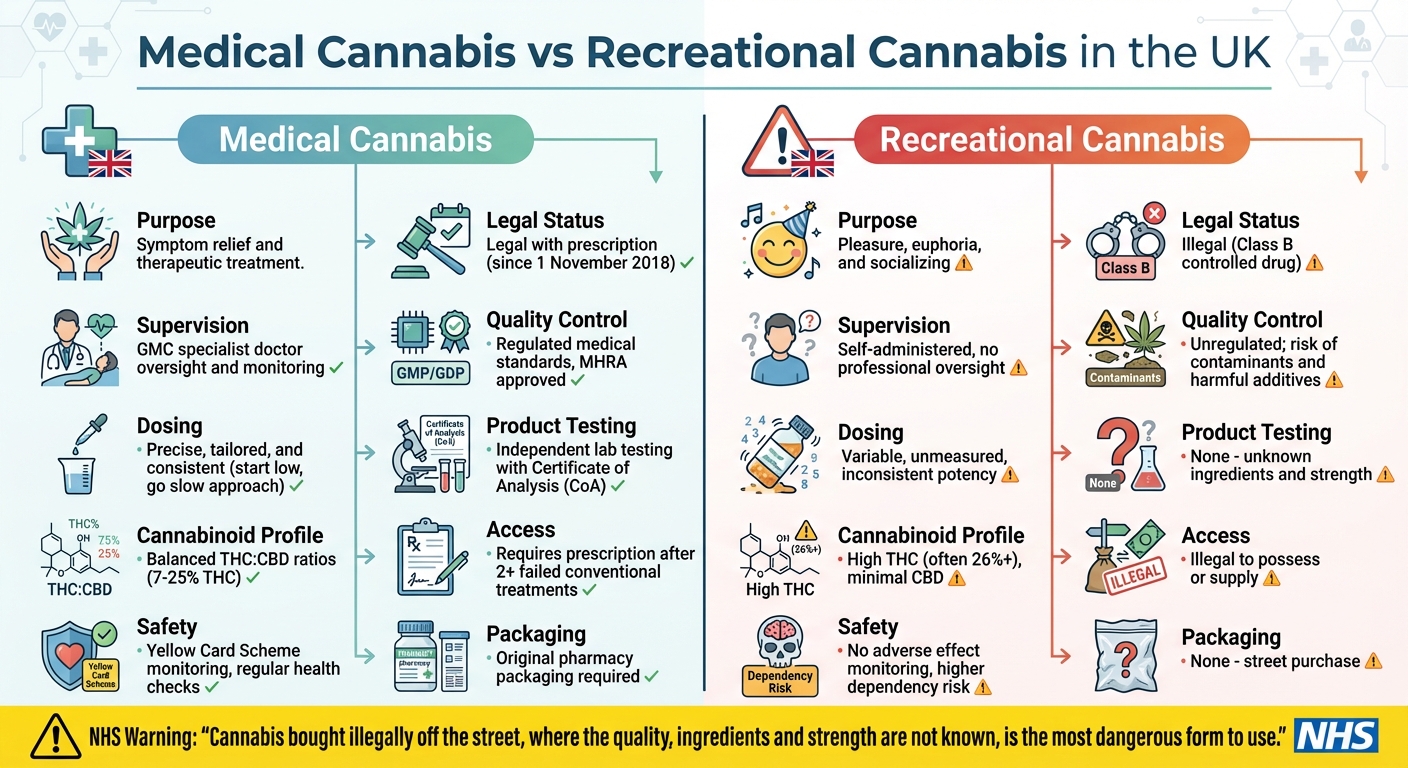
- Purpose: Medical cannabis is used for symptom relief, while recreational cannabis is consumed for pleasure.
- Legal Status: Medical cannabis is legal with a prescription; recreational use is illegal.
- Supervision: Medical use involves specialist doctors and tailored treatment plans; recreational use lacks professional oversight.
- Quality: Medical products meet strict safety standards; recreational cannabis is unregulated and may contain harmful contaminants.
- Dosing: Medical cannabis offers precise dosing; recreational cannabis has inconsistent potency.
Medical cannabis is carefully regulated to ensure patient safety, while recreational cannabis poses legal and health risks due to its unregulated nature.
Medical vs Recreational Cannabis: Key Differences in the UK
Cannabis: Medical vs Street Cannabis: What’s Safe, What Isn’t?
Purpose and Intended Use
The key distinction between medical and recreational cannabis lies in their purpose. Medical cannabis is used as a therapeutic option, prescribed to alleviate symptoms and improve the quality of life for patients dealing with conditions like chronic pain, epilepsy, multiple sclerosis (MS), and anxiety. On the other hand, recreational cannabis is consumed for personal enjoyment, socialising, or achieving a psychoactive "high", with no medical oversight. These differing purposes significantly shape how each is managed and administered, as explored below.
Medical Cannabis for Treatment
In the UK, medical cannabis is generally considered a last-resort treatment, prescribed only after conventional therapies have failed. NHS prescriptions are currently limited to specific cases, such as children and adults with severe epilepsy (e.g., Lennox-Gastaut and Dravet syndromes), adults experiencing chemotherapy-induced nausea, and individuals with MS-related muscle stiffness. Patients must typically have tried at least two other treatments before being eligible for a cannabis-based prescription.
Private clinics, however, may take a broader approach, prescribing medical cannabis for conditions like chronic pain and sleep disorders when standard treatments prove ineffective. Studies indicate that around 33% of medical cannabis users take it daily, highlighting its role in ongoing symptom management. Medical formulations are carefully crafted to balance CBD and THC for therapeutic benefits. As Releaf UK explains:
Think of THC as a key that fits directly into a lock. CBD is more like a hand resting on the thermostat. It doesn’t take over, but it gently adjusts the settings.
Recreational Cannabis for Pleasure
Recreational cannabis use is primarily driven by the desire for enjoyment, relaxation, or stress relief, often with the goal of experiencing the psychoactive effects of THC. Unlike medical use, recreational consumption lacks professional oversight, making it riskier. It also remains illegal in the UK under the Misuse of Drugs Act 1971. Recreational cannabis products typically prioritise THC potency over a balanced composition, often containing lower levels of CBD.
Personalised Care for Medical Patients
Medical cannabis treatment is highly individualised, involving specialist consultations, tailored dosing, and continuous monitoring – features absent in recreational use. In the UK, prescriptions can only be initiated by doctors listed on the GMC Specialist Register, who bear full clinical and medico-legal responsibility. The General Medical Council underscores this:
the decision to prescribe should be based on an assessment of the individual patient.
This personalised approach is crucial for managing risks like psychosis and dependency, which are more likely without clinical oversight. Treatment plans are designed around the patient’s medical history, current medications, and specific needs. Regular health checks, such as liver function monitoring for CBD users, help ensure safety. Additionally, clinical supervision is vital for spotting potential drug interactions, as both CBD and THC can influence how other medicines work.
Elios Clinics exemplify this patient-centric approach, offering services such as eligibility assessments, video consultations with GMC-approved doctors, tailored treatment plans, and ongoing support.
| Feature | Medical Cannabis | Recreational Cannabis |
|---|---|---|
| Primary Goal | Symptom relief and therapeutic treatment | Pleasure, euphoria, and socialising |
| Supervision | Specialist doctor oversight and monitoring | Self-administered |
| Legal Status (UK) | Legal only with a valid prescription | Illegal to possess or supply |
| Dosing | Precise, tailored, and consistent | Variable and unmeasured |
| Quality Control | Regulated medical standards (GMP/GDP) | Unregulated; risk of contaminants |
Legal and Regulatory Framework in the UK
The legal landscape for cannabis in the UK is shaped by its dual roles: a controlled substance for medical purposes and an illegal drug for recreational use. While medical cannabis operates under strict regulations, recreational cannabis remains entirely prohibited and unregulated.
Medical Cannabis: Legal with Prescription
Medical cannabis became legally available in the UK on 1 November 2018, following its reclassification from Schedule 1 to Schedule 2 under the Misuse of Drugs Regulations 2001. This shift acknowledged its potential medical benefits but imposed strict controls. According to the Department of Health and Social Care:
"From 1 November doctors on the General Medical Council’s specialist register will be able to prescribe cannabis-based products for medicinal use, where clinically appropriate and in the best interests of patients."
This regulatory framework means medical cannabis is available only with a prescription from a specialist doctor. Oversight is provided by the Home Office, the MHRA, and NICE, ensuring products meet stringent Good Manufacturing Practice (GMP) standards. Most medical cannabis products fall under the category of "unlicensed specials", meaning they are manufactured to high standards but lack full marketing authorisation like conventional medicines.
However, even with a prescription, smoking cannabis is strictly illegal. The Home Office has made this clear:
"Smoking of cannabis and cannabis-based products for medicinal use in humans continues to be prohibited."
Instead, patients must use alternative methods such as oils, capsules, or vaporised preparations of cannabis flower.
The legal framework for recreational cannabis, however, is entirely distinct and far more restrictive.
Recreational Cannabis: Illegal and Unregulated
Recreational cannabis remains classified as a Class B controlled drug under the Misuse of Drugs Act 1971 and is listed as Schedule 1, meaning it is not recognised as having medicinal value in this context. The NHS reinforces this position:
"The government has no intention of legalising the use of cannabis for recreational (non-medical) use. Possessing cannabis is illegal, whatever you’re using it for. That includes medical use cannabis products, unless these have been prescribed for you."
Without regulation, recreational cannabis is not subject to quality or safety checks. This leaves users exposed to risks such as harmful contaminants, inconsistent THC levels, and potentially dangerous additives.
These contrasting legal frameworks also affect how patients can access medical cannabis.
How to Access Medical Cannabis
Accessing medical cannabis legally requires patients to fulfil specific criteria. They must have a documented diagnosis and evidence that at least two conventional treatments have failed to provide relief.
Prescriptions through the NHS are limited, with around 5,000 issued annually. These are typically reserved for severe conditions such as rare forms of epilepsy (e.g., Lennox-Gastaut or Dravet syndromes), chemotherapy-induced nausea, and muscle spasticity caused by multiple sclerosis. For other conditions, including chronic pain and sleep disorders, private clinics provide a broader range of options. For instance, Elios Clinics offers a streamlined process, including expert assessments, video consultations with GMC-approved doctors, personalised treatment plans, and next-day delivery of prescribed medication.
Patients prescribed medical cannabis must carry it in its original packaging, which includes the pharmacy’s dispensing label. Additionally, they need a copy of their prescription and valid photo ID matching the prescription details. Possession without these documents, even for legally prescribed cannabis, could lead to criminal charges.
sbb-itb-24979b8
Composition, Dosage, and Product Quality
When it comes to medical and recreational cannabis, the differences extend far beyond legal frameworks. The way these products are formulated, tested, and regulated sets them worlds apart. Medical cannabis undergoes pharmaceutical-grade scrutiny, while recreational cannabis is produced without the same stringent safeguards.
Cannabinoid Content: Medical vs Recreational
Medical cannabis is carefully designed with specific THC and CBD ratios to target therapeutic needs. For instance, licensed medications like Epidyolex contain pure CBD with zero THC, while Sativex offers a precise THC:CBD ratio in a spray format, often prescribed for conditions like multiple sclerosis spasticity. These products aim to alleviate symptoms without causing unnecessary psychoactive effects.
On the other hand, recreational cannabis is typically bred for its high THC content to maximise its psychoactive "high". Street cannabis often exceeds 26% THC and contains very little CBD, whereas medical cannabis flower is prescribed with THC levels ranging from 7% to 25%, always with controlled cannabinoid profiles. The unregulated nature of recreational cannabis means users often have no reliable information about the potency or composition of what they’re consuming.
This careful formulation in medical cannabis is the backbone of its precise dosing strategies.
Precise Dosing in Medical Cannabis
Medical cannabis dosing is guided by the principle of "start low, go slow." Specialist doctors typically begin with minimal doses – such as 1–2 puffs from a vaporiser or 2.5–5 mg of oral THC – and adjust gradually based on the patient’s response. Most patients require around 1 gram per day, although some may need up to 5 grams.
In November 2025, the Medical Cannabis Clinicians Society (MCCS) introduced detailed dosing guidelines for 12 conditions, including chronic pain, epilepsy, and anxiety. Dr Rowan Thompson, Vice Chair of the MCCS, highlighted the importance of these guidelines:
"This guide establishes the foundation needed to develop prescribing confidence and experience with cannabis oils."
Medical cannabis comes in consistent forms like oils, capsules, and EU GMP-certified flower, ensuring predictable cannabinoid profiles. In contrast, recreational cannabis often has unknown levels of THC, CBD, and terpenes. Clinicians also consider bioavailability – THC, for example, is around 2.5 times more bioavailable when inhaled compared to oral ingestion.
This level of precision in dosing is only possible due to the strict quality controls in place for medical cannabis.
Quality Control and Safety Standards
Medical cannabis products must meet rigorous standards set by the Medicines and Healthcare products Regulatory Agency (MHRA) or equivalent international bodies. UK licence holders are subject to inspections to ensure compliance with Good Manufacturing Practice (GMP) standards, guaranteeing consistent quality and safety.
Every batch is independently tested using HPLC (High-Performance Liquid Chromatography) to confirm cannabinoid content. These tests result in a Certificate of Analysis (CoA), which serves as verifiable proof of the product’s THC and CBD levels, as well as its purity. Sam North from Releaf UK underscores the importance of this process:
"Every product prescribed… must be tested independently in a laboratory, so patients and doctors can trust that the reported THC level is accurate."
Recreational cannabis, however, lacks this oversight. The NHS warns:
"Cannabis bought illegally off the street, where the quality, ingredients and strength are not known, is the most dangerous form to use."
Unregulated recreational products may contain harmful substances like pesticides, fungicides, or synthetic cannabinoids, which have been linked to severe health risks, including fatalities. Medical cannabis, by contrast, is monitored through the Yellow Card Scheme, allowing patients and healthcare professionals to report adverse effects and ensuring ongoing safety oversight.
Elios Clinics upholds these rigorous standards, sourcing all prescribed medical cannabis from MHRA-approved suppliers to ensure the highest levels of safety and consistency.
Clinical Oversight and Patient Journey
When it comes to medical cannabis, the treatment process is structured and prioritises safety, standing in stark contrast to the risks associated with recreational use.
Medical Cannabis Treatment Pathway
Medical cannabis is never the first option – it’s only considered when other licensed medications have failed to meet a patient’s needs. The journey begins with a specialist doctor registered with the General Medical Council (GMC). These specialists prescribe within their area of expertise – for instance, a paediatric neurologist would handle cases of childhood epilepsy.
The Care Quality Commission outlines the responsibilities of the prescribing doctor:
"The prescribing doctor has responsibility for: prescribing the medicine, overseeing a patient’s care and any follow-up treatment, continuing to monitor the effectiveness and side-effects."
Specialists are required to inform patients that most cannabis-based products are unlicensed, with limited long-term safety data and potential side effects. This transparency allows patients to make informed decisions, often with input from a multidisciplinary team (MDT) to ensure the treatment aligns with their best interests.
After treatment begins, clinicians closely monitor its effectiveness, adjust dosages as needed, and document any adverse effects. Side effects are reported to the MHRA’s Yellow Card scheme. To better understand long-term outcomes, NHS England introduced a national patient registry on 1 April 2022 to track clinical interactions and health impacts.
Elios Clinics adheres to this structured pathway, offering subscription-based care that includes consultations, follow-ups, and continuous monitoring to ensure safe and effective treatment.
This thorough and regulated approach is a world apart from the risks associated with recreational cannabis use.
Risks of Recreational Cannabis
Recreational cannabis use operates without the safeguards of medical oversight, making it a far riskier choice. The NHS has issued a clear warning:
"Cannabis bought illegally off the street, where the quality, ingredients and strength are not known, is the most dangerous form to use."
Without professional guidance, users face a higher risk of dependency due to unknown product quality and potency. Prolonged, unregulated use can lead to serious mental health issues, including psychotic illnesses like schizophrenia. Studies also suggest that chronic exposure to high levels of THC during recreational use may negatively impact brain development and mental well-being.
Unlike clinical settings, recreational users have no system for tracking adverse effects such as hallucinations or suicidal thoughts – risks that medical practitioners actively monitor. Additionally, recreational cannabis possession remains illegal in the UK, with potential legal consequences.
Patient Support and Follow-Up Care
Ongoing support is essential for the safe and effective use of medical cannabis.
This isn’t a one-time prescription – it’s a continuous partnership between the patient and their specialist. Doctors are required to maintain detailed records of all prescriptions and regularly audit their practices to ensure safety. Monitoring for potential interactions between cannabinoids and other medications is also critical.
Elios Clinics provides subscription-based care plans, offering flexibility and convenience. Patients can choose quarterly plans for £60 or monthly plans for £20. These include an initial consultation, four follow-up appointments per year, monthly prescriptions, and access to a patient dashboard for tracking progress.
Patients are encouraged to inform their GP about their treatment to ensure coordinated care. Elios Clinics’ patient-centred model exemplifies the advantages of regulated medical oversight, ensuring that medical cannabis remains a safe and effective treatment option – far removed from the unregulated risks of recreational use.
Conclusion
The differences between medical and recreational cannabis are stark. Medical cannabis is prescribed by GMC-registered specialists and operates under strict legal and clinical guidelines, ensuring safety and efficacy for patients. On the other hand, recreational cannabis remains a Class B drug in the UK – illegal, unregulated, and associated with considerable health risks.
The NHS has highlighted the dangers of unregulated cannabis use:
"Cannabis bought illegally off the street, where the quality, ingredients and strength are not known, is the most dangerous form to use."
Medical cannabis is not just legalised; it is carefully managed to prioritise patient safety. Patients benefit from accurate dosing, regulated product quality, and ongoing monitoring to manage side effects and prevent harmful drug interactions. These safeguards are entirely absent in recreational use.
At Elios Clinics, patients receive personalised treatment plans and continuous support, ensuring medical cannabis is both safe and effective. For those who have not responded to traditional treatments, regulated medical cannabis offers a reliable and tailored alternative – far removed from the uncertainties of recreational cannabis use.
FAQs
Who is eligible for a medical cannabis prescription in the UK?
In the UK, getting a medical cannabis prescription isn’t straightforward – it’s reserved for patients who meet specific requirements. To qualify, you must have a diagnosed medical condition where standard treatments have either failed or caused serious side effects. Conditions commonly considered include chronic pain, severe epilepsy (like Lennox-Gastaut or Dravet syndrome), chemotherapy-induced nausea, and muscle stiffness or spasms linked to multiple sclerosis.
These prescriptions can only be issued by a specialist doctor registered with the General Medical Council (GMC). General practitioners cannot prescribe medical cannabis themselves, but they can refer you to a specialist. The specialist will evaluate your condition and decide if you meet the necessary criteria for this treatment.
For those seeking a smoother experience, Elios Clinics offers services such as eligibility assessments, video consultations with GMC-approved specialists, and tailored treatment plans. They even provide next-day delivery of prescribed medication, ensuring a safe and patient-centred approach every step of the way.
How is medical cannabis regulated to ensure its safety compared to recreational cannabis?
Medical cannabis is tightly controlled to prioritise safety and quality, setting it apart from recreational cannabis. It falls under the Misuse of Drugs Regulations 2001, which categorises cannabis-based medicinal products as Schedule 2 drugs. This classification means they can only be prescribed by GMC-registered specialists or through specific agreements, ensuring their use is carefully monitored. In contrast, recreational cannabis remains a Class B illegal drug, with no regulation over its production or distribution.
To ensure safety, medical cannabis undergoes stringent checks, including potency testing, contaminant screening, and adherence to evidence-based guidelines like NICE’s NG144, which outlines approved uses for conditions such as chronic pain and epilepsy. Private providers, such as Elios Clinics, are overseen by the Care Quality Commission (CQC), ensuring high standards for prescribing protocols, product quality, and patient care. Recreational cannabis lacks these protections, making its use more unpredictable and potentially hazardous.
Why is the balance of THC and CBD important in medical cannabis treatment?
The balance between THC and CBD in medical cannabis plays a key role in determining its therapeutic benefits and potential side effects. THC is the compound that produces psychoactive effects, which can be helpful for issues like pain relief or appetite stimulation. However, it can also lead to side effects such as dizziness or anxiety. CBD, in contrast, does not cause intoxication and can counteract some of THC’s less desirable effects while providing its own benefits, such as reducing inflammation and alleviating anxiety.
Finding the right ratio is essential for tailoring treatment to each patient’s needs. For instance:
- Higher CBD to THC ratios (like 2:1 or 1:1) are often chosen for managing conditions like anxiety or epilepsy, especially when avoiding psychoactive effects is a priority.
- Higher THC ratios might be more suitable for addressing severe pain or muscle spasticity.
At Elios Clinics, doctors take a personalised approach by thoroughly evaluating each patient’s symptoms, medical history, and tolerance levels. This ensures that the treatment plan is both safe and effective.
