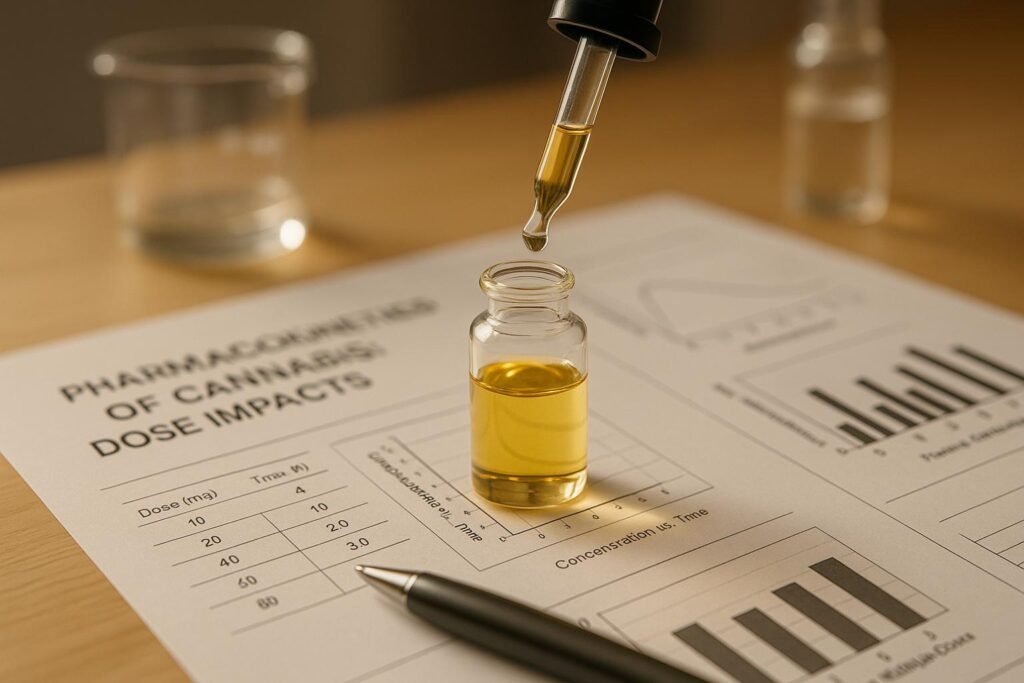
Pharmacokinetics: Cannabis works differently in the body depending on how it’s taken, the dose, and individual factors like age or metabolism. These differences affect how quickly effects start, how strong they are, and how long they last. For example:
- Inhalation: Fastest effects (within 1–10 minutes), lasting 2–4 hours, with 30–50% bioavailability.
- Oral methods: Slower onset (30–90 minutes), effects last 6–8 hours, but with lower bioavailability (4–12% for THC).
- Oromucosal sprays: A middle ground, with effects starting in 15–45 minutes and lasting 4–6 hours.
Cannabinoids like THC and CBD behave differently in the body. THC accumulates in fat tissues, leading to longer-lasting effects in regular users, while CBD has a longer half-life and interacts with other medications more strongly. Factors like genetics, age, and body fat can also influence how cannabis is processed, making personalised treatment plans crucial.
Key points:
- Higher doses often increase effects but not always predictably.
- Advanced formulations, like enhanced capsules, improve absorption and predictability.
- Regular monitoring and dose adjustments are essential for safe and effective treatment.
Clinics in the UK, such as Elios Clinics, focus on tailored cannabis therapies, ensuring safe dosing based on individual needs while working within strict UK standards.
Pharmacokinetics Efficacy & Safety of Novel Selective-dose Cannabis Inhaler in Chronic Pain Patients
Cannabis Delivery Methods and Formulations
The way cannabis is delivered has a big impact on how it works in the body. Each method – whether it’s oral, inhaled, oromucosal, or in capsule form – creates unique patterns in how the body absorbs the cannabinoids, how long it takes for the effects to peak, and how long those effects last. For patients in the UK dealing with chronic pain, mental health challenges, or neurological conditions, understanding these differences is key to getting the best results from treatment.
Oral, Inhalation, Oromucosal, and Capsule Methods
Inhalation methods are the quickest way to experience the effects of cannabis. Whether through vaping or smoking, cannabinoids reach their peak levels in the bloodstream within 3 to 10 minutes, and the effects start almost immediately. This method offers a bioavailability of 30–50%, with effects lasting around 2 to 4 hours.
Oral administration, such as capsules, oils, or edibles, works differently. It takes longer for the effects to kick in – usually between 30 to 90 minutes – and peak levels are reached after 2 to 3 hours. However, the bioavailability is much lower at 4–12% for THC, though the effects last longer, typically 6 to 8 hours.
Oromucosal sprays, applied under the tongue or inside the cheek, strike a balance between the fast action of inhalation and the prolonged effects of oral methods. These sprays peak at concentrations of 2.05–2.58 ng/mL within 1.67 to 2.17 hours. They have a bioavailability of about 13% for THC and 10% for CBD, with effects lasting 4 to 6 hours .
Enhanced capsule formulations, which use technologies like piperine pro-nanolipospheres, are designed to improve oral delivery. These capsules can increase peak concentration by four times (2.1 ng/mL compared to 0.5 ng/mL) and double the total drug exposure. They also reduce the time to peak concentration from 3 hours to just 1 hour. This highlights how advanced formulations can make dosing more predictable and effective.
| Delivery Method | Onset Time | Peak Plasma (Tmax) | Bioavailability | Duration of Effect |
|---|---|---|---|---|
| Inhalation | 1–10 minutes | 3–10 minutes | 30–50% | 2–4 hours |
| Oromucosal | 15–45 minutes | 1.67–2.17 hours | 10–13% | 4–6 hours |
| Oral (standard) | 30–90 minutes | 2–3 hours | 4–12% | 6–8 hours |
| Enhanced capsules | 30–60 minutes | 1.0 hour | Improved | 6–8 hours |
These differences in absorption and effectiveness underline the importance of choosing the right delivery method and formulation for each patient.
How Formulations Affect Dose Predictability
The way cannabis is formulated significantly impacts how reliably patients respond to a given dose. Standard oral formulations often lead to wide variations between individuals, even after steady-state levels are reached. This can make it tricky for healthcare providers to predict doses accurately.
Advanced formulation technologies like self-emulsifying systems and piperine pro-nanolipospheres address this issue. By improving bioavailability and reducing variability, they help achieve faster and higher peak concentrations. This results in more consistent effects and fewer adjustments to dosing schedules.
Chronic use also affects how predictable formulations are. For instance, with CBD, single-dose exposure values of 0.8, 4.5, and 9.9 h×ng/mL have been shown to increase to 2.5, 6.7, and 20.3 h×ng/mL, respectively, during ongoing treatment. This accumulation can enhance the effects over time but requires careful monitoring to adjust doses as needed.
Interestingly, not all cannabinoids behave the same way. Delta-8-THC, for example, builds up in the bloodstream after 14 days of use, whereas THCV levels actually drop by day 14 due to metabolic changes and faster elimination. Additionally, minor cannabinoids like THCV, CBC, CBN, and delta-8-THC, when taken orally, typically reach their peak levels in the plasma and brain within 1.5 to 3 hours.
For patients in the UK, selecting the right formulation is a vital part of successful treatment. Enhanced formulations that provide more predictable dosing can be especially helpful for maintaining consistent symptom relief. It’s important for patients to work closely with their healthcare providers to find the best fit for their needs and treatment goals.
How Dose Affects Pharmacokinetic Parameters
The amount of a cannabinoid consumed influences how it is absorbed, distributed, metabolised, and excreted by the body. These dose-dependent changes impact key pharmacokinetic parameters like peak concentration, time to maximum effect, and elimination rate. However, the specifics vary depending on the type of cannabinoid and the delivery method.
Pharmacokinetics Comparison Across Delivery Methods
Both peak plasma concentration (Cmax) and total drug exposure (AUC) typically increase with higher doses, though the relationship isn’t always perfectly linear. For example, oral CBD demonstrates a clear dose-dependent response. A 20 mg dose results in a mean Cmax of 1.5 ng/mL and an AUC of 6.1 h×ng/mL. When the dose is increased to 60 mg, the Cmax rises to 4.8 ng/mL, with the AUC jumping to 38.9 h×ng/mL. Similarly, single-dose studies show proportional increases in Cmax, with levels of 0.4, 1.2, and 2.2 ng/mL following 5, 10, and 20 mg doses, respectively.
Other cannabinoids, such as delta-8-tetrahydrocannabinol (D8-THC), cannabichromene (CBC), and cannabinol (CBN), also exhibit dose-dependent increases in plasma concentrations and AUC values. This pattern holds true for both single and repeated dosing over 14 days.
| Delivery Method | Dose (mg) | Cmax (ng/mL) | Tmax (hours) | Half-life (hours) | Bioavailability (%) |
|---|---|---|---|---|---|
| Oral THC | 5 | 1.21 | 2.68 | 2.75 | 4–12 |
| Oral CBD | 10 | 2.67 | 0.10 | 4.95 | 6–19 |
| Inhalation THC | 20 | 10–35 | 0.1–0.3 | 1.5–3.5 | 10–35 |
| Oral THCV | 1–10 | 1.5–3 | 1.5–3 | 2–4 | 10–20 |
| Oral CBC | 1–10 | 1.5–3 | 1.5–3 | 2–4 | 10–20 |
Interestingly, the time to reach maximum concentration (Tmax) remains relatively stable across different doses and methods. This consistency helps healthcare providers predict when peak effects will occur, making it easier to plan treatment schedules and advise patients.
Half-life, however, varies significantly depending on the dose and delivery method. For example, CBD has a half-life of 1.4 to 10.9 hours when administered as an oromucosal spray, extends to 2 to 5 days with chronic oral use, and is around 24 hours after a single oral dose. THC shows even more variation, with a half-life of 1 to 3 days in occasional users and 5 to 13 days in chronic users. This difference reflects THC’s tendency to accumulate in fatty tissues due to its lipophilic nature.
Chronic CBD use over nine days shows a marked increase in AUC values, from 0.8, 4.5, and 9.9 h×ng/mL (single dose) to 2.5, 6.7, and 20.3 h×ng/mL. Accumulation patterns also differ by cannabinoid. For instance, D8-THC builds up in plasma after 14 days of repeated oral dosing, while tetrahydrocannabivarin (THCV) shows reduced plasma levels on day 14 compared to day 1, suggesting faster elimination due to metabolic adaptation. These variations underscore the significant individual differences in how cannabinoids are processed.
Individual Differences in Dose Response
Beyond formulation and delivery method, individual factors play a crucial role in cannabinoid pharmacokinetics.
Age is one key factor. Older adults often process cannabinoids more slowly, which may require lower doses or longer intervals between doses to achieve the desired effects. Metabolism also varies widely between individuals. Some people metabolise cannabinoids quickly, reducing their duration of effect, while others metabolise them more slowly, leading to prolonged effects from the same dose.
Body composition further influences cannabinoid behaviour. THC, for example, tends to accumulate in individuals with higher body fat percentages, potentially affecting both how quickly effects begin and how long they last.
Drug interactions also matter. Co-administering cannabinoids can lead to unexpected effects. For example, combining 20 mg Δ9-THC with 640 mg CBD has been shown to amplify subjective effects and impair cognitive and motor functions more than Δ9-THC alone. This interaction arises because CBD inhibits the enzymes (CYP3A4 and CYP2D6) that metabolise THC.
These factors highlight the importance of personalised dosing strategies in medical cannabis treatment. Starting with a low dose and gradually increasing it allows healthcare providers to find the right balance for each patient, reducing the risk of side effects while maximising therapeutic benefits.
Genetic differences may also influence how individuals respond to cannabinoids. Variations in the enzymes responsible for metabolising these compounds could lead to significantly different outcomes from the same dose. However, further research is needed to fully understand these genetic factors.
Regular monitoring and dose adjustments are essential for effective treatment. What works for one person may not be suitable for another, making a tailored approach critical for safe and effective use of medical cannabis.
sbb-itb-24979b8
Factors That Affect Dose Accuracy and Consistency
Achieving consistent dosing with medical cannabis is one of the biggest challenges in clinical practice. Even identical doses can lead to varying responses among patients. These differences arise from a mix of patient-specific characteristics and external factors that influence how cannabinoids are processed in the body. This highlights the importance of tailoring dosing strategies to individual needs.
Patient-Specific Factors
A range of patient-related factors can significantly impact how cannabinoids behave in the body:
- Age plays a major role. As people age, their metabolic clearance slows down, which extends the half-life of THC. Additionally, changes in body fat composition with age can lead to prolonged effects and the accumulation of lipophilic cannabinoids like THC in fatty tissues.
- Genetic variations in CYP enzymes also come into play. Some individuals have genetic polymorphisms that either speed up or slow down cannabinoid clearance, directly affecting the drug’s effectiveness and the risk of side effects. This explains why some patients need higher or lower doses to achieve the same therapeutic results.
- Underlying health conditions can alter how cannabinoids are processed. For example, liver impairment reduces cannabinoid clearance, increasing the risk of accumulation and adverse effects. Similarly, kidney dysfunction can impact the elimination of cannabinoid metabolites. Clinical studies have shown that patients with liver issues experience higher plasma levels and prolonged effects, making careful dose adjustments necessary.
- Concurrent medications can interfere with cannabinoid metabolism. For instance, CBD inhibits the CYP3A4 and CYP2D6 enzymes, potentially increasing the effects or toxicity of other drugs. On the other hand, THC can induce CYP1A2 activity, lowering the levels of medications metabolised through this pathway.
- Body composition matters as well. Patients with higher body fat percentages may experience longer-lasting effects due to increased storage of cannabinoids in fat tissue. This is particularly relevant for THC, which tends to accumulate with repeated use.
These individual factors emphasise the need for personalised dosing and careful treatment planning.
External Factors and Formulation Technologies
Beyond patient-specific traits, external conditions and advancements in formulation technologies also play a key role in ensuring consistent dosing.
- Food intake is a controllable factor that affects cannabinoid absorption. Consuming high-fat meals can significantly boost the bioavailability of oral cannabinoids. For instance, CBD absorption is much higher when taken with food compared to on an empty stomach, leading to increased plasma levels under fed conditions.
- Innovative formulation technologies are helping to improve dose accuracy. For example, pro-nanoliposphere formulations have shown better pharmacokinetic predictability. One study found that a piperine-pro-nanoliposphere oral CBD formulation increased peak plasma concentration (Cmax) by four times and reduced the time to reach maximum concentration (Tmax) compared to standard oromucosal sprays. These technologies help minimise variability by enhancing and standardising absorption.
- Other advancements, such as self-emulsifying drug delivery systems and oromucosal sprays, also improve dose consistency. These methods bypass some of the challenges associated with traditional oral administration, such as variability in gastric conditions and first-pass metabolism.
Proper timing of administration and correct storage conditions are essential for maintaining product integrity and predictable absorption.
Even with these advancements, inter-individual variability in cannabis pharmacokinetics remains a hurdle, particularly with oral formulations that have low bioavailability. This variability underscores the need for precise analytical methods. For example, ultra-high-performance liquid chromatography–tandem mass spectrometry (UHPLC–MS/MS) can help monitor plasma concentrations in clinical settings.
Another layer of complexity arises from metabolic adaptation during repeated dosing. Studies have shown that THCV levels drop by day 14 compared to day 1, indicating increased drug elimination over time. Meanwhile, some cannabinoids, such as D8-THC, and CBD metabolites like 7-COOH-CBD, tend to accumulate with prolonged use.
Clinical Applications for UK Medical Cannabis Standards
In the UK, clinical protocols for medical cannabis have evolved to include rigorous monitoring and tailored treatment adjustments. A key factor influencing these protocols is the significant pharmacokinetic variability among patients. Since individuals respond differently to cannabis-based medicines, delivering effective and safe treatments requires a personalised approach that aligns with strict UK regulatory standards. This variability highlights the need for systematic patient care that adapts to individual differences.
UK medical cannabis standards demand that clinicians consider the wide-ranging differences in how patients absorb and metabolise these medicines. This variability can make standardised dosing protocols less reliable. Oral formulations, in particular, pose challenges due to their generally low bioavailability, which complicates treatment planning and requires careful patient monitoring.
Personalised Treatment Plans and Monitoring
Given the diverse responses among patients, personalised dosing is essential for achieving the best outcomes. For example, studies involving multiple sclerosis patients have shown that maximum daily doses of 22.5 mg THC and 45 mg CBD (administered in three doses) can still result in significant variation in individual responses and pharmacokinetics. To address this, UK medical cannabis standards recommend starting with low doses and gradually increasing them based on how patients respond and tolerate the treatment. Factors like genetics, age, and existing health conditions can lead to vastly different therapeutic outcomes, even with identical doses.
Follow-up appointments every 2–4 weeks are crucial during the initial treatment phase. These check-ins allow for dose adjustments and involve thorough documentation, including patient-reported outcomes, clinical assessments, and, where possible, plasma cannabinoid measurements. Such detailed monitoring helps identify patterns in how patients respond, guiding future dosing decisions.
Capsule formulations are becoming more common in UK practice due to their predictable dosing characteristics. While capsules offer greater consistency compared to other oral methods, clinicians remain attentive to individual variability in patient responses.
This personalised approach to dosing and monitoring lays the groundwork for specialised care, as exemplified by Elios Clinics.
Elios Clinics‘ Role in Patient Care
Elios Clinics takes a patient-focused approach to managing the complexities of pharmacokinetic variability. Eligibility assessments, conducted by GMC-approved doctors, ensure that patients are thoroughly evaluated before starting treatment. These assessments consider factors such as age, concurrent medications, and underlying health conditions that may affect the metabolism of cannabinoids.
The clinic develops customised treatment plans to address the challenges of pharmacokinetic variability. Their medical cannabis specialists work closely with patients to determine the most suitable strain and dosage for their condition. This approach recognises that standardised dosing cannot account for the significant differences in how individuals process cannabinoids.
“We’ll also provide ongoing guidance to help you understand how to use your cannabis effectively and how to monitor any changes in your symptoms.” – Elios Clinics
Education plays a vital role in Elios Clinics’ care model. Patients are guided on how factors such as food intake, timing of doses, and interactions with other medications can influence their treatment outcomes.
Regular follow-ups are a cornerstone of the clinic’s strategy. These appointments allow for tracking patient progress, adjusting treatments, and conducting further evaluations as needed. To ensure continuity of care, Elios Clinics also offers a next-day medication delivery service, which is particularly beneficial given the complexities of maintaining consistent dosing schedules.
Elios Clinics adheres to UK medical cannabis standards by prioritising quality and safety throughout the treatment process. From the initial consultation to follow-up visits, GMC-approved specialists provide continuous support, ensuring that treatments are customised to meet individual needs while complying with regulatory guidelines. Through expert oversight, patient education, and regular monitoring, Elios Clinics exemplifies how UK providers can effectively manage the challenges of cannabinoid pharmacokinetics to deliver safe and effective care.
Conclusion
The way cannabis is absorbed and its effects depend greatly on the method of delivery and the dose. Each route – whether inhalation, oral, or another – comes with its own unique absorption pattern and impact on the body, making careful dose adjustments and monitoring essential.
While higher doses tend to produce stronger effects, the relationship isn’t always straightforward. This unpredictability highlights the difficulty in establishing standard dosing protocols that work universally.
Beyond these pharmacokinetic factors, individual characteristics like age, metabolism, and the use of other medications add another layer of complexity. In response, UK guidelines emphasise starting with low doses, gradually increasing them, and closely monitoring patients. This approach helps account for the variability in how the drug behaves in different individuals.
For example, studies involving multiple sclerosis patients have revealed significant differences in how they respond to treatment, reinforcing the importance of tailoring treatment plans and maintaining regular follow-ups.
Clinics such as Elios Clinics illustrate how a patient-focused, evidence-driven approach can address these challenges. By adhering to UK clinical standards, conducting thorough patient assessments, and providing ongoing therapeutic monitoring, they ensure that medical cannabis treatments are not only safe but also customised to meet the specific needs of individuals dealing with chronic pain, psychiatric conditions, and neurological disorders.
FAQs
How do different cannabis delivery methods affect its effectiveness and how long the effects last?
The way cannabis is consumed plays a big role in how it interacts with the body and how long its effects stick around. For example, inhalation methods like vaping or smoking tend to act quickly, delivering effects almost immediately. In contrast, oral options such as oils or capsules take longer to kick in but often provide effects that last much longer. Then there are topical products, which are usually applied to the skin for targeted relief – these are often non-psychoactive, meaning they don’t produce the “high” typically associated with cannabis.
These differences come down to how the body absorbs and processes cannabis. This not only influences how quickly effects are felt but also impacts how consistent and accurate the dosing can be. By understanding these variations, it’s possible to personalise treatments to better suit individual needs, improving both effectiveness and safety.
How do factors like age and metabolism affect how cannabis is processed in the body?
Individual factors like age, metabolism, and overall health heavily impact how the body processes cannabis – right from absorption to elimination. For instance, older adults with slower metabolisms might find that cannabis stays in their system longer, which could either amplify its effects or extend their duration.
Other elements, such as body weight, liver function, and genetic variations, also influence how cannabis interacts with the body. Being aware of these factors is key to ensuring precise dosing and reliable outcomes, particularly when using medical cannabis for therapeutic treatments.
Why is it important to have a personalised medical cannabis treatment plan?
Personalised treatment plans play a crucial role in ensuring medical cannabis meets the unique needs of each patient. Variables like how cannabis is delivered, the dosage, and the specific formulation can all influence how the body absorbs and reacts to the treatment. This makes a universal approach ineffective.
When treatments are tailored, patients are more likely to achieve steady results, improved symptom relief, and a reduction in unwanted side effects. This method prioritises precision, safety, and the most effective outcomes for each individual’s health condition.