Medical cannabis is gaining attention as a treatment for PTSD, a condition that affects emotional stability and quality of life. Traditional treatments like SSRIs and therapy often fail to provide relief for many sufferers. Cannabis interacts with the endocannabinoid system (ECS), which regulates mood, memory, and stress. Here’s how it helps:
- Reduces hyperarousal: THC binds to CB1 receptors, calming overactive fear responses.
- Improves sleep: THC and CBD help with nightmares and sleep disturbances.
- Eases anxiety: CBD boosts anandamide levels and interacts with serotonin receptors.
- Supports memory processing: Cannabinoids promote extinction learning, helping reframe traumatic memories.
- Stabilises mood: Effective for those with PTSD and depression, tackling multiple symptoms simultaneously.
Studies show noticeable improvements in PTSD symptoms after just three months of cannabis treatment. While side effects like dizziness or fatigue occur in some cases, they are generally mild. Access in the UK requires a PTSD diagnosis and evidence of failed traditional treatments. Clinics like Elios offer consultations, personalised plans, and home delivery, making this option more accessible to those in need.
High expectations: Impact of Cannabis on PTSD Recovery
The Endocannabinoid System and Its Connection to PTSD
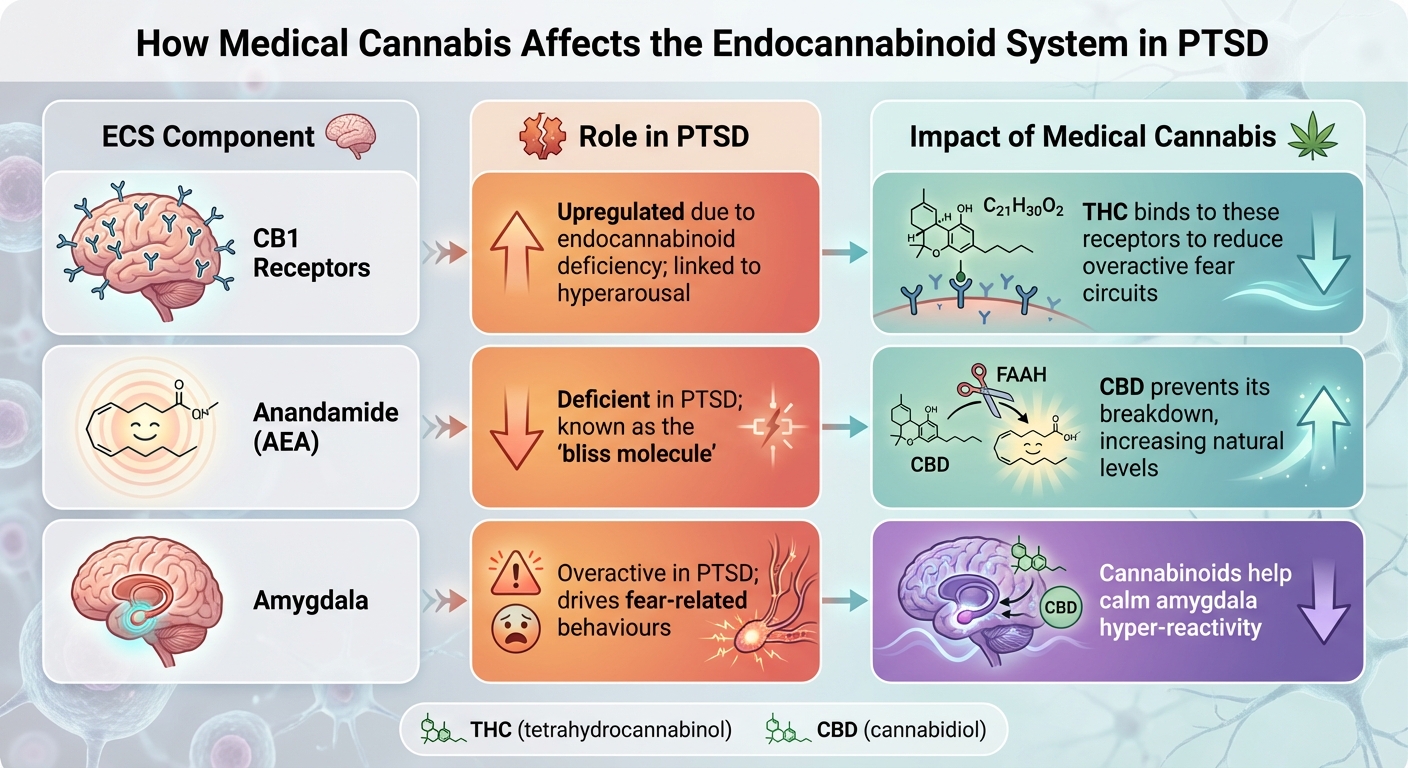
How Medical Cannabis Affects the Endocannabinoid System in PTSD
How the Endocannabinoid System Functions
The endocannabinoid system (ECS) is a key player in maintaining emotional stability. It’s a complex network that influences mood, memory, sleep patterns, and stress responses. The ECS is made up of three core components: cannabinoid receptors (CB1 and CB2), naturally produced endocannabinoids, and enzymes responsible for breaking them down.
CB1 receptors are primarily found in the brain, especially in areas like the amygdala, hippocampus, and prefrontal cortex – regions that are deeply involved in processing fear and traumatic memories. Meanwhile, CB2 receptors are mainly located in the immune system and peripheral nervous system, though they are also present in smaller quantities in the brain.
The body produces two main endocannabinoids: anandamide (AEA), often referred to as the "bliss molecule", and 2-arachidonoyl glycerol (2-AG). Unlike other neurotransmitters, these are not stored for later use – they’re made on demand. Once their job is done, enzymes like FAAH and MAGL break them down.
The ECS plays a critical role in managing stress, largely through its interaction with the hypothalamic-pituitary-adrenal (HPA) axis. Anandamide helps to prevent unnecessary stress responses, acting as a kind of "gatekeeper", while 2-AG assists the body in returning to a calm state after a stressful event. This system operates through retrograde signalling, where endocannabinoids travel backward across synapses to regulate the release of other neurotransmitters such as GABA and glutamate.
How Trauma Disrupts the Endocannabinoid System
Experiencing severe trauma can throw the endocannabinoid system off balance. In individuals with PTSD, anandamide levels drop significantly, leaving the body unable to maintain emotional stability. Research on survivors of the 11th September 2001 attacks revealed that those who developed PTSD had notably lower levels of 2-AG compared to those who didn’t.
To compensate for this shortfall, the brain increases the number of CB1 receptors, a process known as upregulation. However, this adaptation often backfires. The increased availability of CB1 receptors in the amygdala is closely tied to abnormal threat processing, heightened fear, and the hyperarousal symptoms frequently seen in PTSD.
"There is convincing evidence from multiple studies for reduced endocannabinoid availability in PTSD. Brain imaging studies show molecular adaptations with elevated cannabinoid type 1 (CB1) receptor availability." – Alexander Neumeister, M.D., Professor of Psychiatry and Radiology, NYU School of Medicine
This disruption undermines the ECS’s ability to act as a "brake" on stress responses, leading to prolonged and exaggerated reactions to perceived threats. Interestingly, women with PTSD often exhibit more pronounced CB1 receptor upregulation compared to men, which may explain why PTSD tends to affect women more severely and at higher rates. These imbalances open the door for medical cannabis to help restore the system’s equilibrium.
How Medical Cannabis Affects the Endocannabinoid System
Medical cannabis offers a way to address the disruptions in the ECS caused by trauma. Its active compounds – primarily THC and CBD – interact with the ECS to help restore balance. THC, which is structurally similar to anandamide, acts as a partial CB1 agonist, helping to compensate for the body’s reduced levels of this crucial endocannabinoid. This can help reduce fear responses and alleviate symptoms like nightmares.
CBD, on the other hand, works by inhibiting the breakdown of anandamide. It does this by interfering with the enzyme FAAH, effectively boosting the body’s natural levels of the "bliss molecule". Additionally, CBD interacts with serotonin receptors (specifically 5-HT1A), providing further anti-anxiety benefits. Together, these cannabinoids help the ECS better manage stress, fear, and emotional reactions.
| ECS Component | Role in PTSD | Impact of Medical Cannabis |
|---|---|---|
| CB1 Receptors | Upregulated due to endocannabinoid deficiency; linked to hyperarousal | THC binds to these receptors to reduce overactive fear circuits |
| Anandamide (AEA) | Deficient in PTSD; known as the "bliss molecule" | CBD prevents its breakdown, increasing natural levels |
| Amygdala | Overactive in PTSD; drives fear-related behaviours | Cannabinoids help calm amygdala hyper-reactivity |
Medical cannabis also influences memory processes, helping to limit the retrieval of traumatic memories while encouraging extinction learning – the brain’s ability to overwrite fear responses tied to trauma. This dual approach tackles both the biological and psychological effects of PTSD, offering a comprehensive way to manage the condition.
How Medical Cannabis Reduces PTSD Symptoms
Medical cannabis directly addresses core PTSD symptoms by targeting disruptions in the endocannabinoid system (ECS). Research highlights benefits in four key areas: easing fear and anxiety, supporting memory processing, improving sleep, and stabilising mood.
Lowering Fear, Anxiety, and Hyperarousal
One of the standout effects of medical cannabis is its ability to reduce hyperarousal, a hallmark of PTSD. This is achieved by rebalancing the ECS. In PTSD, low levels of anandamide and 2-AG leave the amygdala – our brain’s "fear centre" – in overdrive. THC helps by binding to CB1 receptors, while CBD enhances natural cannabinoid levels, offering additional relief.
A study found that medical cannabis reduced hyperarousal symptoms significantly, with scores dropping from 31.0 to 6.6. Overall PTSD severity, measured by CAPS scores, also saw a dramatic decrease – from 98.8 to 22.5. CBD further supports anxiety relief by interacting with 5HT1A serotonin receptors, producing quick calming effects.
However, dosage matters. Lower doses of THC (around 7.5 mg) have been shown to reduce anxiety, while higher doses (around 12.5 mg) might have the opposite effect. The terpenes in cannabis, such as myrcene and linalool, can amplify these calming effects, working alongside cannabinoids to encourage relaxation and reduce panic.
| Symptom Cluster | Mechanism of Action | Primary Cannabinoid |
|---|---|---|
| Hyperarousal | Balancing the HPA axis and reducing amygdala activity | THC (Low Dose) |
| Anxiety | Interaction with serotonin receptors (5HT1A) | CBD |
| Fear Response | Supporting fear extinction via CB1 receptors | THC & CBD |
| Panic/Stress | Enhanced effects with calming terpenes | Full-spectrum extracts |
This calming effect sets the stage for another powerful benefit: processing traumatic memories.
Helping Process Traumatic Memories
Cannabinoids play a key role in helping patients process traumatic memories. They promote extinction learning, where individuals form new, non-threatening associations with trauma-related cues. CBD is particularly effective in reinforcing these new associations during extinction therapy, while other cannabinoids may interrupt the reconsolidation of traumatic memories, reducing their emotional weight.
"Cannabinoids have been shown to be an effective treatment option for patients with PTSD. Besides aiding to relieve the symptoms and enhance extinction training, they also are relatively well tolerated." – Marika L. Forsythe, Saba University School of Medicine
Cannabis also helps regulate the HPA axis, preventing stress hormones from spiking when patients confront traumatic memories. This memory regulation complements another essential benefit: better sleep.
Improving Sleep Quality and Reducing Nightmares
Sleep problems, including nightmares, are a common struggle for those with PTSD. THC interacts with CB1 receptors to reduce the intensity of nightmares and help patients fall asleep more easily. Meanwhile, CBD’s calming effects counteract the hyperarousal that often disrupts sleep.
Between 2015 and 2018, Dr Nitsa Nacasch and her team at the Brüll Mental Health Centre in Israel treated 14 combat veterans resistant to other treatments with medical cannabis. Over 1.1 years, these veterans saw significant improvements in sleep duration and quality (p < 0.01). The synthetic cannabinoid nabilone has also been shown to either eliminate nightmares entirely or significantly reduce their severity. For example, in one case, a ten-year-old girl with PTSD experienced a drop in sleep disturbance scores from 59 to 38 after five months of treatment with CBD and a sublingual spray.
Stabilising Mood and Improving Daily Life
Medical cannabis doesn’t just tackle individual symptoms – it can also stabilise mood and improve overall daily functioning. PTSD and depression often go hand in hand, with around 77% of PTSD patients also meeting the criteria for major depression. Cannabis appears particularly effective for these individuals, as it works on multiple neurobiological pathways simultaneously. THC addresses ECS deficits, while CBD reduces heightened glutamate activity, which is linked to flashbacks.
These effects translate to better mood and greater ability to engage in everyday life. The dramatic drop in CAPS scores – from 98.8 to 22.5 – mirrors improvements in work, relationships, and overall daily functioning.
"Trauma-related disorders such as PTSD can be considered as disorders of the endogenous (endocannabinoid) systems… Such a deficit might be to some extent rectified by exogenous THC." – Michael T. Lynskey, Drug Science
sbb-itb-24979b8
Research Evidence on Medical Cannabis for PTSD
Results from Patient Studies
Project Twenty21 monitored 238 PTSD patients in the UK between August 2020 and November 2023. Findings, published in March 2024, revealed a decrease in mean PCL-C scores from 58.0 to 47.0 over three months, showing a moderate effect size (Cohen’s d = 0.69).
Another study from the UK Medical Cannabis Registry evaluated 162 PTSD patients, reporting notable improvements in symptoms, sleep quality, and anxiety at 1-, 3-, and 6-month intervals (p < 0.05). Interestingly, 77% of participants screened positive for probable major depression, and those individuals experienced even greater reductions in PTSD symptoms.
"PTSD symptomatology reduced substantially 3 months after commencing treatment… with a significant interaction indicating greater improvement in those with depression." – Michael T. Lynskey et al., Drug Science
Similar outcomes were observed internationally, such as in Tel Aviv’s study on treatment-resistant combat veterans, which supported improvements in PTSD symptoms and sleep quality. These findings lay the groundwork for deeper exploration into the safety of this treatment.
Safety Profile and Side-Effects
While the benefits are promising, understanding potential side-effects is equally important. Medical cannabis appears to be generally well tolerated. In the UK registry study of 162 patients, 20.37% reported adverse events, most of which were mild to moderate. The most common side-effects included insomnia and fatigue (both affecting 12.35% of patients), alongside dizziness, light-headedness, headaches, nausea, and increased heart rate.
"Associated improvements in HRQoL were observed in patients who initiated CBMP therapy. Adverse events analysis suggests acceptability and safety up to 6 months." – UK Medical Cannabis Registry Study Authors
Experts stress the importance of careful titration – starting with low-THC strains and gradually increasing the dose – to reduce risks and find the best therapeutic balance. Notably, in the Israeli veteran study, no cases of misuse or addiction were reported during the follow-up period.
What Research Is Still Needed
Despite encouraging results and a generally favourable safety profile, more rigorous research is essential. Current evidence from randomised controlled trials (RCTs) on cannabis for PTSD is rated as "Low" as of June 2025. Much of the existing data comes from retrospective cohort studies and patient registries rather than gold-standard double-blind, placebo-controlled trials.
"There is a need for high quality, randomized studies of cannabinoids to determine whether cannabis has any effects on PTSD symptoms." – Cannabis Evidence Project
Key areas for further investigation include establishing clear causality, determining optimal dosing strategies, and understanding long-term effects beyond 6–12 months. Variations in THC/CBD ratios and methods of administration add complexity to standardising treatment. Currently, eight clinical trials are underway worldwide, exploring different aspects of cannabis use for PTSD. Additionally, more research is needed on Complex PTSD, as its symptoms – such as dissociation – may respond differently to cannabis compared to standard PTSD.
Getting Medical Cannabis for PTSD in the UK
UK Laws on Medical Cannabis
Since November 2018, medical cannabis has been legal in the UK under the 2018 Regulations. These regulations outline the use of cannabis-based products for medicinal purposes (CBMPs), which are classified as specialist-only medications. This means your GP cannot prescribe them – only doctors registered as specialists with the General Medical Council (GMC) are authorised to do so.
Prescriptions are guided by the NICE guideline [NG144], which includes both licensed medicines like Sativex and Nabilone, as well as unlicensed plant-derived cannabinoids containing THC and CBD. While NICE primarily addresses conditions like chronic pain and treatment-resistant epilepsy, specialists are permitted to prescribe CBMPs for PTSD when standard treatments have not been effective. This framework ensures that access to medical cannabis is carefully regulated and tailored to those who need it most.
Who Qualifies for Medical Cannabis Treatment
To access medical cannabis for PTSD in the UK, patients must meet specific requirements. Firstly, a healthcare professional must confirm a PTSD diagnosis. Secondly, there must be evidence that at least two previous treatments – commonly standard medications like SSRIs or SNRIs, or therapies such as CBT or EMDR – were tried and either failed to provide relief or caused intolerable side effects.
"An individual must have an established diagnosis and evidence of failure of at least two treatment approaches before being eligible to legally receive prescribed CBMPs in the UK." – Project Twenty21
Before booking a consultation, it’s essential to gather your medical records, including a GP-issued Summary Care Record (SCR). This documentation simplifies the eligibility assessment process. Most private medical cannabis clinics in the UK accept direct self-referrals, so a formal GP letter isn’t always necessary. Once eligibility is confirmed, patients can proceed with specialised consultations and treatment.
How Elios Clinics Can Help
For those meeting the criteria, Elios Clinics offers a straightforward route to accessing medical cannabis for PTSD. They start with a free eligibility assessment. If you qualify, a GMC-approved specialist will conduct a video consultation to review your medical history and decide whether CBMPs are a suitable option for you.
If approved, your specialist will design a personalised treatment plan. Elios Clinics provides next-day delivery of your medication straight to your home, ensuring timely access to treatment. They also offer flexible payment options: choose between a monthly plan (£20 per month) or a quarterly plan (£60 per quarter) for a 12-month treatment package. This includes the initial consultation, four follow-up appointments, and monthly prescriptions.
Follow-up appointments, typically scheduled every three months, allow your specialist to monitor your progress, fine-tune dosages, and address any concerns. This regular oversight ensures your treatment remains both safe and effective throughout the process.
Conclusion: A New Approach to Managing PTSD
For the 4% of the UK population living with moderate to severe PTSD, medical cannabis offers a new avenue for treatment. Unlike traditional methods that often focus on masking symptoms, medical cannabis interacts directly with the body’s endocannabinoid system – the very system disrupted by trauma. With psychotherapy dropout rates remaining high, cannabis-based medicinal products provide an alternative for those who feel they’ve run out of options.
The benefits go beyond symptom management. Data from the UK registry, involving 162 PTSD patients, revealed notable improvements in anxiety and sleep at 1-, 3-, and 6-month intervals. These changes translate into better daily functioning, improved mood, and more restful nights.
"Cannabinoids have been shown to be an effective treatment option for patients with PTSD. Besides aiding to relieve the symptoms and enhance extinction training, they also are relatively well tolerated." – Marika L. Forsythe and Andrew J. Boileau
What sets medical cannabis apart is its ability to address multiple symptoms at once. By reducing hyperarousal, improving sleep, easing intrusive thoughts, and supporting the brain’s ability to process traumatic memories, it offers a comprehensive approach to healing. For those resistant to traditional treatments, nearly 80% reported overall improvement after starting medical cannabis – a success rate that conventional pharmacotherapy struggles to achieve. These findings underline its potential as a practical and effective treatment option.
Elios Clinics builds on this promise by providing accessible, evidence-based care. Through a free eligibility assessment, consultations with GMC-approved specialists, personalised treatment plans, and next-day medication delivery, they ensure patients receive timely and effective support. With flexible payment plans starting at just £20 per month and follow-up care every three months, patients can safely optimise their treatment. For those left disappointed by conventional methods, medical cannabis offers not just relief but a real chance to regain control over their quality of life.
FAQs
How does medical cannabis help manage PTSD symptoms?
Medical cannabis works by engaging with the body’s endocannabinoid system – a complex network of receptors responsible for regulating functions like mood, memory, and stress. Compounds found in cannabis, such as THC and CBD, interact with two key receptors, CB₁ and CB₂, to help restore balance within this system.
This interaction can help diminish the over-consolidation of traumatic memories, assist the brain in reducing fear responses, and ease symptoms like hyper-arousal and anxiety. By soothing these stress-related pathways, cannabis offers a potential source of relief for individuals coping with PTSD.
What side effects might medical cannabis have when used to treat PTSD?
Medical cannabis can be an option for managing PTSD symptoms, but it’s not without potential side effects. Commonly reported issues include dry mouth, dizziness, changes in appetite, drowsiness, and difficulties with memory or concentration. Some people may also experience increased anxiety or paranoia, nausea, or even vomiting. Though rare, long-term or heavy use can lead to conditions like cannabis hyperemesis syndrome, which involves persistent vomiting.
Another point to consider is that high-THC strains might increase your heart rate and could interact with certain medications. If you’re thinking about using medical cannabis, it’s essential to consult a healthcare professional to ensure it’s the right choice for you.
Who can access medical cannabis treatment for PTSD in the UK?
In the UK, people diagnosed with moderate to severe PTSD might qualify for medical cannabis treatment. To access this, an evaluation and prescription from a specialist doctor authorised to prescribe cannabis-based medicines are required.
Eligibility is assessed individually, and medical cannabis is generally considered when standard treatments have proven ineffective or are not appropriate. If you think medical cannabis could help with your PTSD symptoms, it’s worth discussing this with a qualified healthcare professional to understand your options.