Cancer pain can be debilitating, and finding the right treatment is crucial for improving quality of life. Opioids are a long-established option, providing strong pain relief but with serious risks like addiction, overdose, and severe side effects. Medical cannabis is emerging as an alternative, offering milder side effects and potential benefits for managing pain, anxiety, and sleep issues.
Key Points:
- Opioids: Effective for severe pain but carry risks like dependency, respiratory depression, and gastrointestinal side effects.
- Medical Cannabis: May reduce pain intensity and symptom burden, with fewer severe risks, though evidence varies across studies.
- Combination Therapy: Some research suggests using both may lower opioid doses, but clinical evidence is limited.
- UK Access: Medical cannabis is legal via specialist prescriptions but rarely available on the NHS. Private clinics, like Elios Clinics, offer tailored support.
Quick Comparison:
| Aspect | Medical Cannabis | Opioids |
|---|---|---|
| Effectiveness | Moderate pain relief; mixed evidence | Strong for severe pain |
| Side Effects | Dizziness, drowsiness, dry mouth | Constipation, addiction, overdose |
| Risks | Low dependency risk (under supervision) | High risk of dependency, overdose |
| Discontinuation Rate | 11% (6-month study) | 10-20% (due to side effects) |
Choosing between these treatments depends on individual needs, medical history, and tolerance for risks. Always consult a healthcare professional for personalised advice.
Medical Cannabis vs Opioids for Cancer Pain: Side-by-Side Comparison
How Effective Are Medical Cannabis and Opioids for Cancer Pain?
Medical Cannabis: Pain Relief and Patient Outcomes
Research into medical cannabis for cancer pain shows a mixed bag of results, with some promising findings but also notable limitations. For example, a six-month study highlighted that medical cannabis significantly reduced certain measures of oncology pain. Yet, controlled trials often paint a more nuanced picture. A Phase 3 trial of Sativex found it no better than a placebo for pain relief in advanced cancer patients. Similarly, a trial using a 1:1 THC:CBD oil reported only a slight pain reduction (0.85 units), which fell below the threshold considered clinically relevant, and noted additional psychomimetic side effects.
Earlier studies, however, provide some encouraging insights. Back in 1975, a pilot study revealed that 20 mg THC oil capsules delivered significant pain relief compared to a placebo for advanced cancer patients (P<0.05). Fast forward to 2010, another study demonstrated that nabiximols significantly improved mean pain scores (P=0.024) and reduced the need for breakthrough pain medications (P=0.004). These findings suggest that while medical cannabis may not always outperform standard treatments, it does hold potential for certain patients.
Opioids: The Established Standard for Cancer Pain
Opioids have long been the go-to treatment for severe cancer pain, particularly in palliative care, where they are essential for managing chronic or neuropathic pain in advanced cancer stages. However, despite their widespread use, the evidence supporting opioids is not as robust as one might expect. Many studies are outdated, involve small participant groups, or report adverse event rates ranging from 11% to 77%. Even with these shortcomings, opioids remain widely prescribed due to their long-standing track record and well-documented mechanisms of action.
Comparing Clinical Trials
When comparing cannabis and opioids head-to-head, the results are mixed. A 1975 study found no significant difference in pain relief between 10 mg of THC and 60 mg of codeine, suggesting that a modest dose of THC could match the pain-relieving effects of a standard opioid dose. However, more recent systematic reviews bring additional nuance. One review of randomised trials concluded with high certainty that adding medical cannabis to opioid therapy had little to no effect on pain relief for chronic cancer pain patients.
These findings highlight that both treatments are assessed not just for their ability to relieve pain but also for their side effects and overall impact on patient well-being. This broader evaluation is critical for guiding treatment choices and balancing efficacy with safety.
Safety and Side Effects: Medical Cannabis vs. Opioids
Common Side Effects of Medical Cannabis
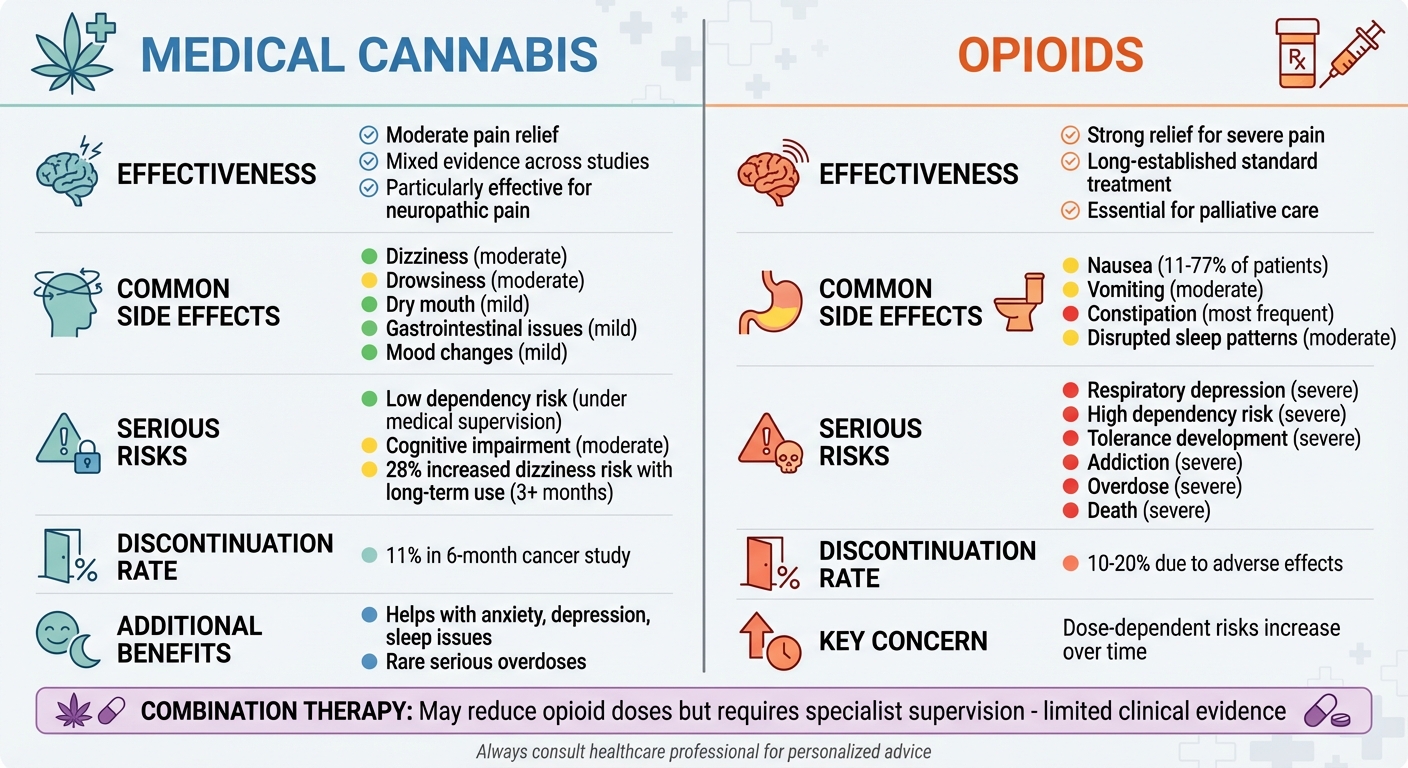
Medical cannabis tends to come with milder side effects compared to opioids, but regular monitoring is still essential. The most commonly reported issues include dizziness, drowsiness, dry mouth, and fluctuations in blood pressure – both increases and decreases. Some patients also report digestive problems such as nausea, vomiting, or abdominal discomfort.
It can also affect cognitive functions like learning, memory, and attention, and may increase the risk of mood disorders. Studies highlight that long-term use raises certain risks. For example, trials lasting three months or more showed a 28% increased risk of dizziness, compared to just 9% in shorter studies. In a six-month study involving cancer patients, 11% stopped using medical cannabis due to side effects like fatigue, dizziness, hallucinations, unpleasant taste, and drowsiness.
The likelihood of dependency on medical cannabis is considered "probably small" when usage is carefully managed by a specialist doctor. However, the risk rises with higher THC concentrations. Illegally sourced cannabis carries the greatest risk due to uncertainties about its quality, composition, and potency.
Opioid Side Effects and Risks
In contrast, opioids come with a much harsher side effect profile. Nausea and vomiting are reported by 11% to 77% of patients, while constipation is the most frequent complaint. Beyond these uncomfortable symptoms, opioids pose severe, life-threatening risks such as respiratory depression, which can be critical.
Long-term opioid use raises additional red flags, including tolerance (needing higher doses for the same effect), dependency, and the risks of addiction, overdose, and death. These dangers are dose-dependent, meaning they become more pronounced as dosages increase over time. Between 10% and 20% of patients discontinue opioid treatment due to adverse effects. For chronic non-cancer pain, medical cannabis was associated with fewer treatment discontinuations due to side effects compared to opioids (OR 0.55, 95% CrI 0.36 to 0.83).
Side Effects Comparison Table
| Treatment Type | Common Side Effects | Serious Risks | Discontinuation Rate |
|---|---|---|---|
| Medical Cannabis | Dizziness, drowsiness, dry mouth, gastrointestinal issues, mood changes | Dependency risk (low under medical supervision), cognitive impairment | 11% in a 6-month cancer study |
| Opioids | Nausea (11-77%), vomiting, constipation | Respiratory depression, tolerance, dependency, addiction, overdose, death | 10-20% due to adverse events |
The table highlights a stark contrast between the two treatments. While both have side effects, opioids carry significantly more severe and potentially fatal risks. Medical cannabis, though not without its concerns – especially regarding cognitive effects and dependency – generally presents a more tolerable option for many patients when used under proper supervision.
Using Medical Cannabis to Reduce Opioid Doses
Medical Cannabis as an Opioid-Sparing Treatment
Medical cannabis might help lower the amount of opioids needed to manage cancer-related pain. Research on animals has shown that combining delta‑9‑THC with opioids can enhance pain relief. However, clinical trials have yet to provide strong evidence supporting this effect. Many of these studies kept patients on their usual opioid doses, making it difficult to fully explore whether cannabis could genuinely reduce opioid use. As a result, the certainty of evidence for this opioid-sparing potential remains very low. Still, this possible interaction opens the door for further research into using both treatments together.
Benefits of Using Both Treatments Together
The idea of combining medical cannabis with opioids brings a few potential advantages. Lab studies suggest that cannabinoids might extend pain relief and reduce the amount of opioids needed. However, as with any treatment, balancing effectiveness with safety is critical. While this combination could lead to better pain control and less reliance on opioids, it may also increase the risk of side effects like nausea, vomiting, or even misuse. For cancer patients already using opioids, introducing medical cannabis should always involve specialist supervision. Given the limited clinical evidence, any changes to pain management plans should be carefully discussed with a healthcare professional to monitor both benefits and risks.
sbb-itb-24979b8
What UK Patients Should Know About Medical Cannabis
Legal Status and Access in the UK
In the UK, medical cannabis falls under the classification of a Class B drug as per the Misuse of Drugs Act 1971. This means its possession, production, and supply are generally illegal. However, since November 2018, specialist doctors have been allowed to prescribe cannabis-based medicines. Despite this change, the government has firmly stated that cannabis will not be legalised for recreational use.
Patients with a valid prescription can legally possess cannabis-based medicinal products without needing a licence from the Home Office. However, prescriptions via the NHS are rare and typically reserved for severe conditions. For those suffering from conditions like cancer pain, private specialist clinics are often the main route for obtaining medical cannabis. Smoking cannabis remains unlawful, except in research settings. Given these strict regulations, seeking professional advice is crucial for safe and legal access.
How Elios Clinics Supports Patients
Elios Clinics provides a streamlined approach for cancer pain patients seeking medical cannabis as part of a broader pain management plan. The process begins with a free eligibility assessment to evaluate whether treatment is appropriate. Patients then have video consultations with GMC-approved doctors, who personalise treatments based on their medical history and needs. The clinic also ensures convenience with next-day medication delivery and a patient dashboard for managing prescriptions and appointments. Regular follow-ups help doctors monitor progress and adjust dosages, offering tailored support, especially for patients transitioning from opioid use.
Cost and Accessibility
Accessing medical cannabis treatment in the UK is primarily a private healthcare option, as NHS prescriptions for conditions like cancer pain are exceedingly rare. To make treatment more affordable, Elios Clinics provides flexible payment plans. Patients can opt for a Quarterly Subscription at £60 per quarter or a Monthly Subscription at £20 per month, both adding up to £240 annually. For those who prefer flexibility, the Pay As You Go option costs £50 per session, covering initial and follow-up consultations. Repeat prescriptions within the agreed care plan are free, though adjustments outside the plan incur a £30 fee. Additionally, patients can request a medical cannabis travel letter for £10, ensuring they can travel with their medication when needed.
Choosing the Right Pain Management Approach
Key Takeaways
When it comes to managing cancer pain, both medical cannabis and opioids have their own strengths and drawbacks. Opioids are highly effective for moderate to severe cancer pain, but they come with serious risks, including dependency, overdose, and side effects like constipation, nausea, and disrupted sleep patterns. Meanwhile, medical cannabis offers a safer profile, with serious overdoses being extremely rare. It’s particularly effective for relieving neuropathic pain, which can be challenging to treat.
Beyond pain relief, medical cannabis can also help alleviate symptoms like anxiety, depression, and sleep issues. Its side effects tend to be less severe compared to the broader range of adverse reactions linked to opioid use. Interestingly, combining medical cannabis with opioids may allow for effective pain control while reducing the risks associated with higher opioid doses.
Ultimately, the choice between opioids, medical cannabis, or a combination of both depends on factors like the type of pain, your medical history, tolerance for side effects, and personal comfort with treatment risks. This highlights the importance of tailoring pain management to each individual’s unique needs.
Patient-Focused Care with Elios Clinics
Personalised support is key to finding the right treatment, and Elios Clinics is here to help if you’re considering medical cannabis for cancer pain management. Their GMC-approved doctors work closely with your healthcare team to create treatment plans tailored specifically to your needs.
Elios Clinics offers a free eligibility assessment to help you determine if medical cannabis is a suitable option. With flexible subscription plans, next-day delivery, and a user-friendly patient dashboard, they combine convenience with top-notch clinical care. For patients looking to reduce their reliance on opioids, Elios Clinics provides a supportive and accessible pathway to explore alternative pain management strategies.
Does Cannabis/Marijuana Work for Pain and Can it Replace Opiates?
FAQs
How do medical cannabis and opioids differ in managing cancer pain?
Medical cannabis and opioids are both used to manage cancer-related pain, but they function differently and come with their own sets of advantages and risks. Opioids are known for their effectiveness in treating severe pain and providing quick relief. However, they often bring along side effects like constipation, nausea, drowsiness, and, in some cases, dependence or even respiratory depression. Medical cannabis, by contrast, provides milder pain relief but is frequently used alongside opioids to lower the required dosage, which can help reduce opioid-related side effects.
Cannabis tends to have a gentler side-effect profile, with issues such as dry mouth or dizziness being relatively mild and short-lived. It’s particularly useful for managing chronic or neuropathic pain and can be a good option when opioids alone cause intolerable side effects. While opioids are typically reserved for acute or intense pain, medical cannabis is often introduced for long-term pain management or to target specific symptoms.
For those considering medical cannabis as part of their treatment plan, Elios Clinics provides personalised care. Their services include consultations with GMC-approved doctors and next-day medication delivery, ensuring a safe and patient-centred approach to managing pain.
Can medical cannabis help reduce reliance on opioids for managing cancer pain?
Research suggests that medical cannabis may play a role in reducing the reliance on opioids for managing cancer-related pain. Evidence points to cannabis having opioid-sparing effects, which means patients might need lower doses of opioids when cannabis is used as part of their treatment plan.
This combination could help lessen the side effects tied to high-dose opioid use, offering a more balanced and potentially safer way to manage pain. That said, it’s crucial to work closely with a healthcare professional to find the most suitable approach for your individual needs.
How can patients in the UK legally access medical cannabis for managing cancer pain?
In the UK, patients dealing with cancer-related pain can legally obtain medical cannabis through a prescription from a specialist doctor. This typically requires an eligibility assessment, which is often conducted via a video consultation with a GMC-approved doctor.
Clinics like Elios Clinics offer a range of services, including customised treatment plans and next-day delivery of prescribed medication. Their approach prioritises safety, high-quality care, and a personalised experience for patients.