Accessing medical cannabis in the UK is possible but comes with strict rules. Since 2018, specialist doctors can prescribe cannabis-based medicinal products (CBMPs) under specific conditions. However, the process involves detailed documentation, eligibility checks, and adherence to controlled drug regulations.
Key Points:
- Who can prescribe? Only GMC-registered specialists in private clinics or NHS hospital consultants (for limited conditions).
- Eligibility: Patients must have tried and failed conventional treatments for conditions like chronic pain, epilepsy, or multiple sclerosis.
- Prescription rules: Valid for 28 days, with medication stored in original containers. Patients must carry photo ID and prescription proof.
- NHS vs Private Clinics:
- NHS: Limited conditions (e.g., severe epilepsy, MS spasticity), long waiting times, and fewer prescriptions (under 100 since 2018).
- Private clinics: Broader access, faster consultations (1–2 weeks), and tailored treatments, but patients bear the cost (£250+ annually).
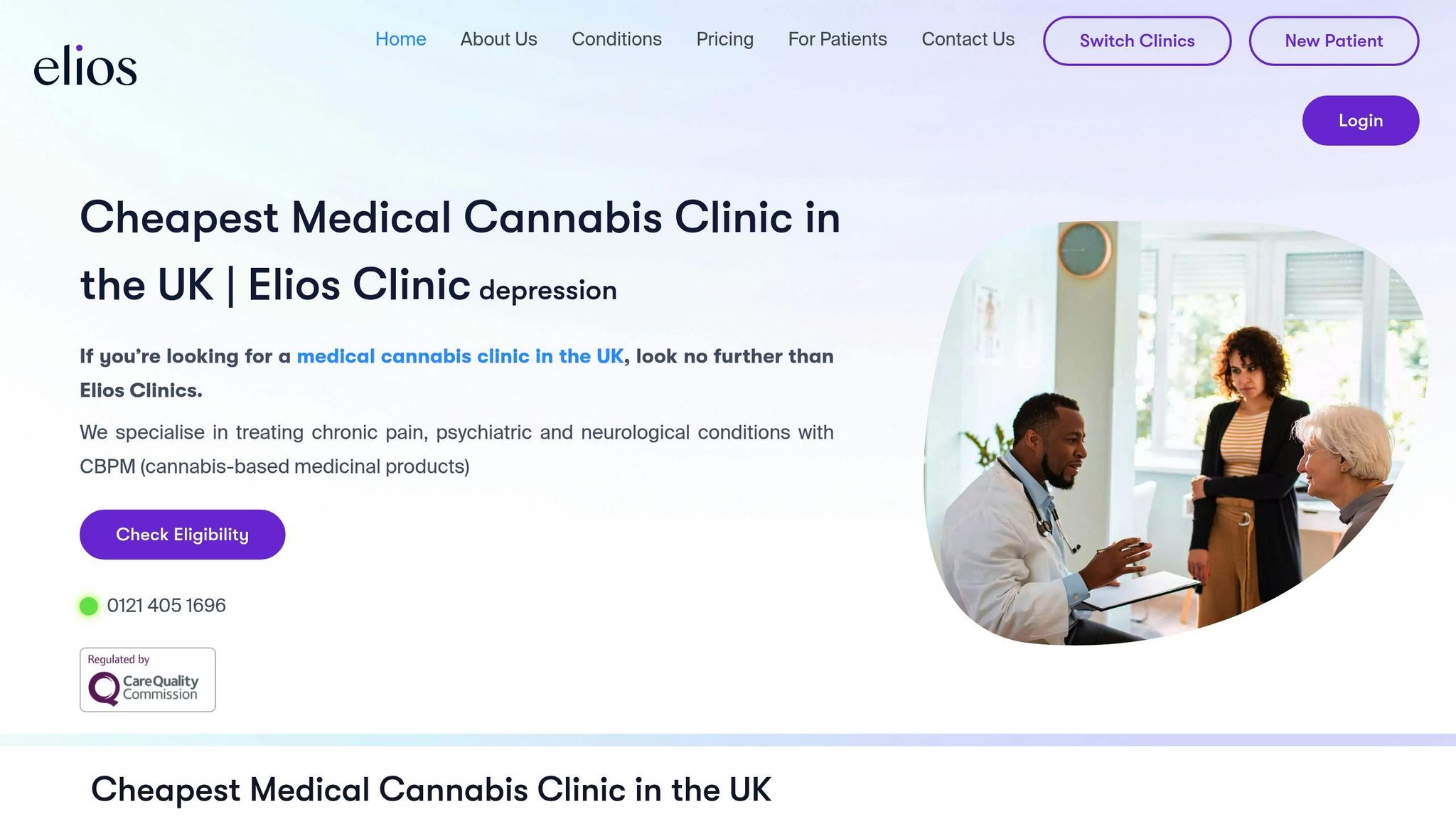
Private clinics like Elios Clinics streamline the process with video consultations, next-day medication delivery, and patient education, offering a more accessible pathway for those seeking alternative treatments.
Why is it so difficult to get medicinal cannabis in the UK? – BBC News
UK Medical Cannabis Legal Framework
In the UK, medical cannabis – known as Cannabis-Based Medicinal Products (CBMPs) – can only be prescribed by doctors who are registered with the General Medical Council (GMC). These specialists are authorised to prescribe CBMPs strictly in situations where traditional treatments have not worked.
This ensures that CBMPs are used as a last resort, prioritising patient safety and maintaining a high standard of care.
Patient Eligibility and Prescription Process
Patient Eligibility Requirements
In the UK, patients can only be prescribed cannabis-based medicinal products (CBMPs) after standard treatments have been tried and proven ineffective.
Eligible patients typically include those with chronic pain, epilepsy, multiple sclerosis, or specific psychiatric conditions. To confirm eligibility, a detailed medical history and an assessment by a doctor registered with the General Medical Council (GMC) are mandatory. These specialists are responsible for determining whether medical cannabis is a suitable treatment option.
Consultation and Documentation Requirements
Comprehensive documentation is a critical part of the process. Before any consultation, patients must provide specific documents to confirm their eligibility and identity.
Medical records play a central role. Patients need to submit their full medical history, including GP notes, hospital discharge summaries, and specialist reports, to demonstrate that conventional treatments have not worked.
Additionally, a government-issued photo ID, such as a passport or driving licence, is required to verify identity. Patients must also sign a treatment agreement with their chosen clinic, which outlines the terms of care and the legal responsibilities involved.
These steps ensure a structured and compliant process for both patients and clinics.
How Private Clinics Handle Prescriptions
Private clinics have developed efficient systems to meet these requirements while offering faster access to treatment compared to the NHS. Operating under Care Quality Commission (CQC) standards, these clinics ensure full compliance with UK regulations.
Consultations are often conducted via video appointments with GMC-registered specialists. During these sessions, doctors review the patient’s medical history, evaluate their current condition, and decide whether CBMPs are appropriate. Specialists document their clinical reasoning for prescribing medical cannabis, creating a clear and lawful record.
Once a prescription is issued, the medication is supplied in pharmacy-labelled containers, complete with all necessary identification details. This ensures patients receive their treatment safely and in line with legal standards.
sbb-itb-24979b8
NHS vs Private Medical Cannabis Access
When it comes to medical cannabis, the divide between NHS and private healthcare systems becomes stark, particularly in terms of accessibility and patient experience.
Limited NHS Medical Cannabis Access
Access to medical cannabis through the NHS is restricted to a very narrow range of conditions. Currently, prescriptions are mainly available for severe childhood epilepsy syndromes like Dravet syndrome and Lennox-Gastaut syndrome, chemotherapy-induced nausea and vomiting, and muscle spasticity in multiple sclerosis.
This limited scope stems from the NHS’s reliance on extensive clinical trial evidence before approving treatments. The National Institute for Health and Care Excellence (NICE) guidelines further constrain access, effectively excluding patients dealing with conditions like chronic pain, anxiety, PTSD, and other ailments that might otherwise qualify for cannabis-based treatments.
Adding to the challenge, NHS prescriptions can only be issued by hospital consultants. Many consultants, however, remain hesitant due to the limited clinical data available and concerns about professional liability. As a result, fewer than 100 NHS prescriptions have been issued since 2018, despite growing demand from patients.
Private Clinic Advantages for Patients
Private clinics, while operating under the same regulatory framework, provide far broader access to medical cannabis treatments. These clinics can prescribe cannabis-based medicinal products (CBMPs) for a wide range of conditions where standard treatments have failed, including chronic pain, fibromyalgia, anxiety disorders, PTSD, and inflammatory conditions.
One of the key advantages of private clinics is the speed of access. While NHS patients may face waiting times of several months or longer for specialist appointments, private clinics often arrange consultations within a matter of days or weeks. Many also offer video consultations with GMC-registered specialists, removing geographical barriers and making the process far more convenient.
Private clinics also excel in tailoring treatments to individual needs. Specialists can adjust dosages, switch formulations, and refine treatment plans based on how patients respond – flexibility that is often difficult to achieve within the NHS framework. Additionally, private clinics offer a much wider range of products, including CBD and THC formulations in various forms such as oils, capsules, and flower products. This variety allows for precise dosing and better symptom management.
The following table highlights the key differences between NHS and private access to medical cannabis:
NHS vs Private Access Comparison
| Aspect | NHS Access | Private Clinic Access |
|---|---|---|
| Eligible Conditions | Severe epilepsy, chemotherapy side effects, MS spasticity | Broad range where conventional treatments failed |
| Prescribing Doctors | Hospital consultants only | GMC-registered specialists |
| Typical Wait Time | 6–12 months or longer | 1–2 weeks |
| Consultation Format | In-person hospital appointments | Video consultations available |
| Treatment Cost | Free (prescription charges apply) | £250 annually |
| Product Range | Very limited formulary | Wide range of CBD/THC products |
| Follow-up Care | Limited ongoing support | Routine follow-ups |
| Prescription Volume | Under 100 since 2018 | Thousands of active patients |
The cost of private treatment is often a sticking point. While NHS care is free at the point of delivery, private treatment involves ongoing expenses. However, many patients find the personalised care, faster access, and broader treatment options worth the investment, especially when NHS treatments have failed to address their needs.
Continuity of care is another area where private clinics stand out. They offer structured pathways with regular follow-up appointments, ensuring that treatments can be optimised over time. In contrast, NHS patients often struggle to maintain consistent access to prescribing specialists, making it difficult to adjust treatments as needed.
Elios Clinics: Patient-Focused Medical Cannabis Care
Elios Clinics blends strict adherence to UK medical cannabis laws with a commitment to accessible and patient-centred care. Founded by Dr. Kam Lally and Dr. Attam Singh, the clinic operates within private healthcare, offering a seamless pathway for those seeking alternative treatments.
Comprehensive Patient Services
Elios Clinics addresses the challenges many face accessing medical cannabis through the NHS by offering a streamlined, patient-focused service. The clinic starts with free eligibility assessments, removing the financial hurdle that often discourages patients from exploring this treatment option.
Consultations are conducted via video with GMC-approved doctors, ensuring accessibility regardless of location. These sessions are designed to create personalised treatment plans, taking into account each patient’s medical history, current medications, and unique symptoms.
One feature that sets Elios Clinics apart is its next-day delivery service for prescribed medications. This quick turnaround eliminates the delays often associated with traditional pharmacy systems, ensuring patients receive their treatment without unnecessary frustration.
The clinic provides specialised care for individuals managing chronic pain, psychiatric conditions, and neurological disorders – areas where NHS criteria can sometimes fall short. By offering these services, Elios Clinics bridges the gap for patients in need of alternative solutions.
Quality, Safety, and Patient Education
Elios Clinics doesn’t just meet legal requirements – it goes a step further by prioritising the quality of its cannabis-based medicinal products (CBMPs). Each product is carefully sourced to meet pharmaceutical standards, addressing the variability in cannabis treatments and ensuring consistent dosing.
Patient education is another cornerstone of the clinic’s approach. Many individuals prescribed medical cannabis receive little guidance on its proper use, potential side effects, or how it interacts with existing medications. Elios Clinics provides detailed education, covering safe usage, legal considerations, and realistic expectations for treatment outcomes.
The clinic also collaborates with general practitioners and other healthcare providers to ensure medical cannabis treatments are seamlessly integrated into a patient’s overall care plan. This teamwork enhances safety and keeps all providers informed about prescribed treatments.
Elios Clinics Features and Benefits
Elios Clinics offers flexible payment plans and robust support systems, ensuring accessibility for all patients:
| Service Component | Cost | Features | Coverage |
|---|---|---|---|
| Quarterly Subscription | £60 per quarter | Initial consultation, 4 follow-ups, monthly prescriptions, patient dashboard | 12-month treatment pathway (£240 total) |
| Monthly Subscription | £20 per month | Initial consultation, 4 follow-ups, monthly prescriptions, patient dashboard | 12-month treatment pathway (£240 total) |
| Pay As You Go | £50 per session | Assessment and treatment plan design | Initial consultation only; follow-ups extra |
| Follow-up Consultations | £50 per session | Treatment monitoring and dose adjustments | Individual appointments as needed |
| Repeat Prescriptions | £0–£30 | Online prescription requests 24/7 | Free within care pathway; £30 for changes |
| Travel Documentation | £10 per letter | Travel letters for legal compliance | Supports international travel needs |
The patient dashboard offers a digital hub where individuals can track prescriptions, manage appointments, and maintain records for regulatory purposes. This tool simplifies administration, allowing patients to focus on their health.
For those travelling, the clinic provides documentation to confirm the legal use of prescribed medical cannabis, easing the complexities of international travel.
Regular follow-up consultations ensure treatments remain effective and compliant with regulations. These sessions allow doctors to adjust dosages, refine treatment plans, or address side effects, ensuring the best possible outcomes for patients.
Conclusion: Understanding UK Medical Cannabis Prescription Laws
The legal framework for medical cannabis in the UK took a significant turn in 2018, allowing GMC-registered specialists to prescribe cannabis-based medicinal products (CBMPs) after amendments to the Misuse of Drugs Regulations 2001. Today, most prescriptions are issued through private clinics, with thousands of patients now accessing treatment. However, the cost can be steep, with some patients paying as much as £2,000 per month.
This shift has enabled the development of care models that prioritise patients while adhering to legal requirements. Private clinics, such as Elios Clinics, have made the process more accessible by offering streamlined assessments, video consultations, and comprehensive patient education. At the same time, the regulatory environment continues to adapt, providing clearer guidelines and improved safety standards across the sector.
FAQs
What are the main differences between getting medical cannabis on the NHS and through private clinics in the UK?
Accessing medical cannabis through the NHS in the UK remains challenging because of strict regulations and highly restrictive prescribing guidelines. NHS prescriptions are typically reserved for rare cases, leaving many patients without suitable treatment options.
Private clinics have emerged as a more accessible alternative, offering quicker appointments, a broader range of treatments, and greater prescribing flexibility. However, this convenience comes at a cost, with patients generally spending between £80 and £300 per month for private treatment. For many individuals, these clinics have become the main way to obtain medical cannabis in the UK.
How do clinics like Elios Clinics provide safe and regulated access to medical cannabis in the UK?
Clinics such as Elios Clinics play a crucial role in providing safe, regulated access to medical cannabis, strictly following UK laws like the Misuse of Drugs Regulations 2001 (amended 2018). These laws are in place to ensure that controlled substances are prescribed and dispensed with patient safety as the top priority.
Elios Clinics operates under the watchful eye of the Care Quality Commission (CQC) and relies exclusively on GMC-approved doctors for prescribing treatments. This ensures that every prescription is not only legally compliant but also tailored to the patient’s needs. By refining their processes, they make treatments accessible more efficiently, all while maintaining high standards of care and safety.
What do I need to qualify for a medical cannabis prescription in the UK?
To obtain a medical cannabis prescription in the UK, you’ll need an evaluation by a specialist doctor who is authorised to prescribe cannabis-based treatments. This assessment involves a thorough review of your medical history, current health condition, and any previous treatments to determine whether other options have failed or are not suitable for your needs.
If you meet the criteria, the doctor will submit a prescription request. This request is then carefully reviewed under strict UK regulations to ensure that medical cannabis is prescribed only when it is deemed clinically appropriate and safe for you as a patient.